A Breath of Not-So-Fresh Air: the Combined Effects of Air and Noise Pollution
Blog post by Jasmin Skinner
As of 2022, more than 55% of the world’s population reside in urban settings, with that number expected to rise to 80% by 2050 (1). As a direct consequence, more than 4.3 billion people are exposed to pollution daily, often from multiple sources simultaneously. Particulate matter (PM), or air pollution, is thought to be responsible for approximately 8.8 million deaths per year, and this is without even considering the exacerbation of respiratory and cardiovascular diseases such as asthma and arrhythmia (2). While the health effects of air pollution have been well documented, few studies have evaluated the combined effect of air and noise pollution. As PM exposure rarely occurs in isolation, assessing the combined impact of several types of pollutants on health provides a more realistic and accurate depiction of the impact of urban living; with this knowledge becoming increasingly important as urban centers densify.
In this blog, we discuss a recent publication from Kuntic et al., in which they provide one of the first reports on the adverse health effects of both simultaneous and individual exposure of mice to aircraft noise and airborne PM. The authors specifically focused on how these pollutants affect the murine cerebro-pulmonary-cardiovascular axis, and what gene regulatory effects were observed within these organ systems (3).
This webinar features Dr. Emma Karey as she presents evidence of the first- and second-hand exposure risks of vaping, discusses how public perceptions influence e-cigarette usage, and provides a translational framework for integrating scientific principles and novel conditions. WATCH NOW
Study Parameters and Protocol
Kuntic et al., first compared three standardized National Institute of Standards and Technology (NIST) PM mixtures: diesel particles (NIST1), urban atmospheric PM (NIST2), and fine PM of less than four micrometers in diameter (NIST3). This comparison was intended to determine which PM mixture most closely reproduced pathophysiological effects observed in urban settings. The results of the pilot study indicated that NIST2 most reliably reproduced detrimental effects and was thus used for the main study (3).
To evaluate the putative additive effects of exposure to PM and noise, 172 male mice were divided into 4 groups: PM only, noise only, PM and noise, and fresh air with no noise. Mice were exposed to the various test conditions for approximately six hours per day during their natural rest period for three consecutive days. The PM concentration used was approximately 200μg/m3 and equivalent to that observed in highly polluted cities. Blood pressure was measured during these procedures using a non-invasive tail cuff; after three days, tissues from the heart, brain, and lung tissues were extracted for protein expression analysis. Additionally, retinal, cerebral, and aortic vasculature were extracted to determine vascular function post-procedure (3).
How does pollution affect the respiratory system?
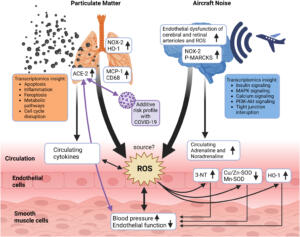
As expected, the effects of particulate matter were most pronounced in the lungs, primarily as a consequence of tissue inflammation and oxidative damage. Oxidative stress increased in all exposure groups, but was notably greatest in the co-exposure group, and was associated with increased expression of NADPH oxidase (NOX-2) and heme oxygenase-1 (HO-1), enzymes involved in the regulation of oxidative stress and inflammation.
In addition to the inflammatory response, pulmonary ACE-2 was upregulated in the co-exposure group. This observation suggests that air pollution may act as a cofactor in increasing the risk of COVID-19 mortality, in part by facilitating viral entry into cells through upregulation of ACE-2 expression. Additionally, PM exposure was found to be the main factor responsible for gene regulatory effects, affecting cellular processes including apoptosis, ferroptosis, phagosome and lysosome activation, as well as triggering antioxidant and metabolic stress responses (3).
How does pollution affect the central nervous system?
Unsurprisingly, the effects of noise pollution were most evident in the brain. Cortical activation and release of the stress hormones adrenaline and noradrenaline were significantly elevated in the noise group, with a similar trend observed in the PM+noise group. The release of adrenaline and noradrenaline can result in vascular and cerebral inflammation as well as oxidative stress, which, over time, can increase the likelihood of diabetes, high cholesterol, hypertension, and eventually cardiovascular disease. Additionally, protein expression of NOX-2 and P-MARKS were upregulated by noise alone, with a synergistic increase in the co-exposure group.
Noise pollution was also responsible for gene regulatory effects. Neuroactive ligand-receptor interaction, insulin, and MAPK signaling were differentially modulated from noise alone, whereas co-exposure affected PI3K and calcium signaling, as well as tight junction regulation. In addition, impairment of cerebral and retinal vascular function accompanied by increased cerebral oxidative stress was observed in all exposure groups, with exposure to PM and noise pollution resulting in an additive effect (3).
How does pollution affect the cardiovascular system?
The cardiovascular system was equally affected by both kinds of pollutants, with the greatest effect observed in the co-exposure group. Interestingly, just a single exposure to either air or noise pollution induced a notable disruption in endothelial function, albeit to a lesser degree than the impairment observed with co-exposure. Regardless of exposure, all three test groups experienced a significant increase in both systolic and diastolic blood pressure, but surprisingly did not experience any additive effects from co-exposure.
Both air and noise pollution independently induced remarkably distinct regulatory effects in the aorta. Air pollution was primarily responsible for affecting the regulation of cell growth factors, PI3K/MAPK/Wnt/Ras/TNF signaling, and lysosomal activation and endocytosis. On the other hand, noise pollution was primarily responsible for affecting the regulation of mTOR/HIF-1/PPAR/AMPK signaling, the citric acid cycle, apoptosis, oxidative phosphorylation, and peroxisomes. Interestingly, after a single co-exposure, only marginal parts of these changes in gene regulation were observed (3).
Figure 1: Potential pathophysiological mechanism following individual or co-exposure of air pollution (urban atmospheric particulate matter, NIST2) and noise pollution (air craft take-off landing noises). © 2023 Kuntic et al., licensed under CC BY 4.0.
What do these results mean?
While co-exposure exacerbated inflammation and oxidative stress within the lungs, PM exposure was responsible for a substantial portion of that response. The ultrafine particles within PM are capable of reaching terminal bronchioles, embedding themselves in lung tissue, causing the effects described above. These particles will often be phagocytosed, as cells and organelles aid in the clearance of pathogens and other foreign material. The smallest particles can also enter the bloodstream and the brain via the olfactory nerves, promoting endothelial dysfunction and hypertension, as well as potentially triggering atherosclerotic processes via the bloodstream.
On the other hand, the effects of noise pollution were most apparent in the brain, inducing cardiovascular complications as a result of an increase in circulating stress hormones and phagocytic NOX-2 (3, 5). Notably, the vascular and cerebral microvascular impairment induced by aircraft noises was almost completely prevented by NOX-2 knockout and HO-1 activation, demonstrating the importance of these proteins in mediating noise-induced health effects.
The stress response to aircraft noise increased blood pressure by activating the hypothalamic-pituitary-adrenal (HPA)-axis, a mechanism that mediates numerous physiological processes such as metabolism and immunity (4). As isolated noise pollution exposure already substantially increased blood pressure, air pollution may have been precluded from increasing blood pressure further due to physiological limitations.
As an intermediary between many other organ systems, the circulatory system was unsurprisingly affected by both air and noise pollution. Oxidative stress and inflammation from the lungs and circulating stress hormones promoted the development of endothelial dysfunction and hypertension.
Clinical implications and concluding remarks
This study demonstrates the importance of investigating the individual and simultaneous effects of environmental stressors such as noise and air pollution. When studying these stressors separately, the combined effect of co-exposure is not considered and the health risks of these pollutants may therefore be severely underestimated. Given the global population’s increasing concentration in urban centers, studies such as these are critical to better understanding the potential health impacts of various pollutants. Since particulate matter and aircraft noise are only a subset of the various environmental stressors that affect human health, more holistic approaches such as that presented here are requisites for a comprehensive appreciation of the health impact of environmental factors.
About the Author
About the Author

Jasmin Skinner is an undergraduate student at the University of Western Ontario completing a Specialization in Biology and a Minor in Chemistry, with focused interest in applying these concepts to environmental conservation. As a lover of the outdoors and the arts, much of her time is spent in nature and within the local London art community, creating and connecting with all walks of life. After graduating, she hopes to continue her passion of finding unconventional solutions to environmental issues by working with nature, not against it.
References
- Venditti B. This chart shows the impact rising urbanization will have on the world [Internet]. [place unknown]: World Economic Forum. 2022 Apr [cited 2023 Mar 10]. Available from: https://www.weforum.org/agenda/2022/04/global-urbanization-material-consumption/#:~:text=Today%2C%20more%20than%204.3%20billion,construction%20of%20human%2Dbuilt%20environments.
- United States Environmental Protection Agency [Internet]. Washngton, DC, USA: United States Government; 2023 Mar. Health and Environmental Effects of Particulate Matter (PM); 2022 Aug [cited 2023 March]; Available from: https://www.epa.gov/pm-pollution/health-and-environmental-effects-particulate-matter-pm.
- Kuntic M, Kuntic I, Krishnankutty R, Gericke A, Matthias O, Junglas T, et al.
Co-exposure to urban particulate matter and aircraft noise adversely impacts the cerebro-pulmonary-cardiovascular axis in mice. Redox Biol [Internet]. 2023 Feb;59:102580. Available from: https://www.sciencedirect.com/science/article/pii/S2213231722003524. doi: 10.1016/j.redox.2022.102580 - Sheng JA, Bales NJ, Myers SA, Bautista AI, Roueinfar M, Hale TM, et al. The hypothalamic-pituitary-adrenal axis: development, programming actions of hormones, and maternal-fetal interactions. Front Behav Neurosci [Internet]. 2021 Jan;14:601939. Available from: https://www.frontiersin.org/articles/10.3389/fnbeh.2020.601939/full#:~:text=A%20major%20component%20of%20the,autonomic%20nervous%20system%20(ANS). doi: 10.3389/fnbeh.2020.601939
- Singel KL, Segal BH. NOX2-dependent regulation of inflammation. Clin Sci (London) [Internet]. 2017 Jul;130(7), 479–490. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5513728/. doi: 10.1042/CS20150660