Chronological Age vs Biological Age: Can Aging be Reversed?
Blog post by Jasmin Skinner
While our chronological age is on a fixed trajectory, biological age is a far more variable determination of health. Two individuals could be born simultaneously, but their bodies and subsequently, their cells, could be vastly different in age due to a variety of life circumstances. Disease, drug treatment, lifestyle changes, and environmental exposures have all been observed to influence biological age, however, these changes are not absolute (1,2). Interest in the malleability of biological age has been increasing as the technology and information capable of measuring biological age have improved substantially (3,4). Additionally, as human longevity has been steadily increasing since the turn of the last century, understanding the mechanisms behind age-related illnesses has become an increasingly significant public health dilemma (2,3). Having a simplified summary of one’s current health status could prove extremely beneficial for both health care professionals and individuals alike, but how does one measure their biological age?
Dr. Sam Sternberg describes a new CRISPR-Cas9 paradigm relying on nuclease-deficient bacterial transposons that catalyze RNA-guided integration of mobile genetic elements into the genome. The discovery of a fully programmable, RNA-guided transposase lays the foundation for kilobase-scale genome engineering with broad applications for developing cell and gene therapies. WATCH HERE
How do you measure biological age?
DNA methylation (DNAm) clocks are the primary way to measure one’s biological age, as methylation of specific pairs of nucleotides predictably change as one ages chronologically. Methylation is a long term regulator of epigenetic gene expression; by transferring a methyl group on cytosine, it can recruit or inhibit proteins from binding to DNA, thereby preventing transcription. The most frequently methylated cytosines are those that precede a guanine nucleotide, known as CpG sites. As methylation of these CpG sites occurs at a predictable rate, DNAm clocks are able to produce a measure of biological age and morbidity/mortality risk, based on both CpG methylation and other phenotypic measures of aging (1,5).
Since the advent of the first human DNAm clock, a variety of mouse and improved human DNAm clocks have been developed. The first generation of DNAm clocks sought to simply identify physiological markers of aging, while also attempting to approximate an individual’s chronological age based on their epigenetics (1). Second-generation human DNAm clocks vastly improved upon earlier models by integrating numerous phenotypic and biochemical measurements of aging, which are then compared to the individual’s chronological age to get an estimate of their true biological age (4). This has allowed researchers to develop specialized clocks that are better equipped to assess a particular age-related parameter, such as future age prediction, age-related functional deterioration, or disease-related progression (4). However, each DNA methylation clock is calibrated differently, and could yield different estimates of biological age, depending on the clock used (1).
Can biological age be changed?
As measurements of biological age can fluctuate quite significantly, the question arises of whether biological age is truly a fixed number, or something capable of fluctuating throughout one’s lifetime. Recent reports of biological age reversal in particular disease states, such as diabetes mellitus, have shown promise as appropriate diabetic treatment effectively reduced biological age (6). Additionally, a methylation-supported diet and lifestyle change demonstrated up to an 11-year decrease in age, showing the significant potential for altering biological age (7). Given the intertwined nature of chronic stress and accelerated aging, Poganik et al. sought to investigate fluctuations in biological age, in both a murine model and using clinical data, to further elucidate the variability of biological age in response to a variety of physiological stressors (1,8).
Methodology for determining biological age in physiologically stressed mice
In the mouse model experiments, parabiosis was used, in which two mice were surgically attached resulting in a shared circulatory system. This method has been previously shown to reduce DNA methylation age in murine models, and can provide insight as to how the circulatory system affects biological age (1). To evaluate interactions between blood and age, heterochronic (3 month old and 20 month old) mouse pairs were compared to isochronic (2 three-month-old mice) pairs. Mice were surgically attached and maintained for three months, after which point a subset was euthanized for analysis, and the other subset were surgically separated and allowed to recover for 2 months before euthanization and analysis. Additionally, to determine the impact of pregnancy on biological age, male and female mice were housed together and, after successful pregnancy and birth, pups were euthanized to allow the female mice to recover without needing to nurse (1).
In the human studies, DNA methylation data was obtained from blood samples, or from publicly available human methylation datasets. For the COVID-19 study, blood samples were obtained from individuals who were admitted to an intensive care unit in Boston, Massachusetts. These blood samples were centrifuged to derive a buffy coat from which DNA methylation profiling could be performed. To further elucidate whether physiological stress affects biological age, methylation data from pregnant patients, as well as patients undergoing elective and emergency surgery was obtained from the NCBI Gene Expression Omnibus (GEO), a publically funded genomics data repository, as well as from a few academic collaborators. In addition to the DNA methylation analysis, metabolite and gene expression profiling analysis was performed in a variety of different organs to provide additional data for determining biological age (1).
How did heterochronic parabiosis affect biological age?
After comparing mouse DNA methylation data to the methylation expected at their chronological age, it was determined that heterochronic parabiosis brought about a reversible increase in biological age in the liver, heart, brain, kidney, and adipose tissue of the younger mouse. This was further validated by an increase in gene expression signatures of aging and age-related metabolites that disappeared upon recovery, demonstrating a transient increase in biological age at both a transcriptomic, metabolomic, and DNAm level (1).
These reversible changes were also investigated in pregnant mice, as this highly physiologically stressful event results in several hallmarks of aging, including increased incidence of age-related diseases like heart disease or diabetes. Blood sample testing revealed that biological age increased after mice became pregnant, and decreased after birth, further validating that biological age temporarily increases in response to physiological stress (1).
How does biological age change during pregnancy and surgery?
In all pregnancy datasets, which consisted of a variety of American and European individuals, biological age increased in pregnant humans up until delivery, at which point it significantly decreased. This is consistent with the author’s studies in mice, highlighting the evolutionarily conserved fluctuations in biological age in response to physiological stress. Human patients experiencing major surgery were also evaluated to examine the effects of stress-induced biological aging. While both elective and emergency surgeries are stressful, the physiological impact of an unexpected major surgical event proved to be far more impactful. Patients that received elective surgery experienced a lessened increase in biological age than those that underwent emergency surgery. This was likely due to the underlying reason for surgery, as emergency surgeries tend to occur when their physiological state is critically compromised, which would in turn result in greater physiological stress. Patients who received emergency surgery had a strong and rapid increase in biological age that returned to baseline in the days following surgery, further proving that physiological stress results in a flexible change in biological age (1).
In addition to the pregnancy and surgery cohorts, the authors also sought to determine whether a severe infectious disease like COVID-19 would cause similar fluctuations. Previous studies have reported that individuals with an advanced biological age are more vulnerable to severe cases of COVID-19. The elderly are also up to 90-fold more susceptible to death from COVID-19, demonstrating a connection between biological age and the incidence and severity of COVID-19. To determine how biological age markers fluctuate throughout the course of infection, longitudinal blood samples from patients with COVID-19 were obtained and separated by sex. While different DNA methylation clocks displayed varying results, severe infectious diseases like COVID-19 were observed to reversibly increase biological age, despite the nuanced results that appeared to be both sex- and clock-specific (1).
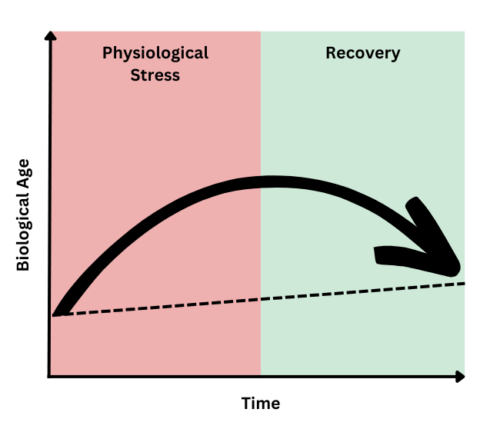
Biological age can increase and decrease, so what?
While the results obtained from Poganik et al. are preliminary and not a recommendation for anti-aging treatment, they highlight a fascinating novel physiological phenomenon. The pattern of stress exposure resulting in an increase in biological age was observed in both mice and human participants, indicating an evolutionarily conserved mechanism in response to both pregnancy and other physiologically stressful events. This temporary increase in biological age could prove useful in drug discovery, as these changes in methylation could be used to predict anti-aging interventions. Additionally, the impact of stress on overall mortality and morbidity cannot be ignored, as severe physiological stress clearly demonstrated an ability to, albeit temporarily, increase one’s biological age. Likewise, biological age may prove to be an asset in the research and characterization of physiological stress and its recovery (1, 8).
Figure 1: Pattern of biological aging and recovery after experiencing physiological stress. Original image inspired by graphical abstract from Poganik et al., 2023.
Limitations of DNA methylation clocks and future directions
While DNAm clocks are currently the most powerful tool to estimate biological age, additional biomarkers and orthogonal approaches are required to truly validate biological age as a predictor of mortality. Additionally, the authors highlight that these fluctuations in biological age could be a result of another yet-to-be identified component of the stress immune response, but also that this is unlikely to be the case. As the DNAm data were consistent with transcriptomic and metabolomic levels, and also were consistent between mice and human participants experiencing pregnancy and surgery, it is very likely that this phenomenon is a result of the physiological stress response (1). However, future work will need to identify whether the successful recovery of biological age results in improved clinical outcomes, or whether this is just a hallmark of the physiological recovery in response to severe stress.
About the Author
About the Author

Jasmin Skinner is an undergraduate student at the University of Western Ontario completing a Specialization in Biology and a Minor in Chemistry, with focused interest in applying these concepts to environmental conservation. As a lover of the outdoors and the arts, much of her time is spent in nature and within the local London art community, creating and connecting with all walks of life. After graduating, she hopes to continue her passion of finding unconventional solutions to environmental issues by working with nature, not against it.
References
- Poganik JR, Zhang B, Baht GS, et al. Biological age is increased by stress and restored upon recovery. Cell Metab. 2023;35(5):807-20.E5. doi: 10.1016/j.cmet.2023.03.015
- Lohman T, Bains G, Berk L, Lohman E. Predictors of biological age: the implications for wellness and aging research. Gerontol Geriatr Med. 2021;7:23337214211046419. doi: 10.1177/23337214211046419
- Crimmins EM, Thyagarajan B, Kim JK, Weir D, Faul J. Quest for a summary measure of biological age: the health and retirement study. Geroscience. 2021;43(1):395-408. doi: 10.1007/s11357-021-00325-1
- Bell CG, Lowe R, Adams PD, et al. DNA methylation aging clocks: challenges and recommendations. Genome Biol. 2019;20:249. doi: 10.1186/s13059-019-1824-y
- Moore LD, Le T, Fan G. DNA methylation and its basic function. Neuropsychopharmacology. 2013;38:23-38. doi: 10.1038/npp.2012.112
- Cortez BN, Pan H, Aguayo-Mazzucato C. DNA methylation supports accelerated biological age in Type 2 diabetes which can be reversed with pharmacological treatments: retrospective cohort study. bioRxiv. 2022;9(14):507908. doi: 10.1101/2022.09.14.507908
- Fitzgerald KN, Campbell T, Makarem S, Hodges R. Potential reversal of biological age in women following an 8-week methylation-supportive diet and lifestyle program: a case series. 2023;15(6):1833-9. Aging (Albany NY). doi: 10.18632/aging.204602
- Yergorov YE, Poznyak AV, Nikiforov NG, Sobenin IA, Orekhov AN. The link between chronic stress and accelerated aging. Biomedicines. 2020;8(7):198. doi: 10.3390/biomedicines8070198