Long-Term Cardiovascular Symptoms of Mild COVID-19
Blog post by Jasmin Skinner
Although the SARS-CoV-2 pandemic has been ongoing for more than two years, a clear understanding of the symptoms of long COVID-19 remains elusive. In this blog post, we review a recent study published in Nature Medicine that investigated cardiovascular symptoms in individuals with prior mild SARS-CoV-2 infections [1].
Common complaints of long COVID
Muscle weakness, fatigue, difficulty sleeping, anxiety, depression, and severely impacted pulmonary diffusion capacities are all common complaints six months post-infection [2]. However, many of the studies examining the long-term effects of COVID-19 have focused primarily on patients who were previously hospitalized [2]. While these individuals have likely experienced the most severe symptoms, only 5.5% of all COVID cases in the United States have resulted in hospitalization, underlining the need for additional research on the long-term effects of mild COVID [3].
Join Augusto Montezano, PhD, as he discusses his research into the role of endotheliitis and ACE2 interactions with COVID-19, and the long-term cardiovascular effects of this inflammation. WATCH NOW
Study overview and baseline characteristics of the cohort
To investigate cardiovascular symptoms of mild COVID, Puntmann et al. selected participants who had contracted COVID-19 but were not hospitalized, and had no known cardiac conditions or comorbidities. A group of individuals who had not contracted the virus served as controls. Subjects were evaluated using a standard questionnaire, blood sampling, and cardiac magnetic resonance imaging at a median of 109 days after initial COVID diagnosis. At this baseline evaluation, roughly 73% of participants reported varying cardiac symptoms that were not present prior to SARS-CoV-2 infection. Symptoms were relatively mild in a majority of the participants, with the most common being shortness of breath. Individuals reporting cardiac symptoms also had significantly higher myocardial native T1 mapping values compared to asymptomatic individuals. Additionally, previously infected individuals were found to have both higher diastolic blood pressures and myocardial mapping values compared to controls.
Lingering cardiac symptoms following mild COVID-19
Follow-up assessments were performed at a median of 329 days after COVID-19 diagnosis. Although 20% of the cohort were asymptomatic at follow-up, 53% of subjects remained symptomatic, and an additional 5% of previously asymptomatic participants had developed new cardiac symptoms. Compared to men, women were more likely to experience continued cardiac symptoms with the most commonly reported being shortness of breath, palpitations, and chest pains. Shortness of breath was often related to an exaggerated tachycardic response and fatigue following exercise. Many participants also experienced some level of exercise intolerance; those most affected often refrained from leaving their homes due to the sudden onset of physical weakness, dizziness, or in rare cases, blackouts.
Although myocardial mapping values generally improved across the entire cohort, native T2 values remained higher in individuals with persistent cardiac symptoms. Participants who were previously infected with SARS-CoV-2 exhibited higher mapping measurements, increased pericardial involvement, and more non-ischemic scarring compared to controls. These findings suggest that cardiac inflammation may be shared among individuals with COVID-19, regardless of the presence of cardiac symptoms. Although the mechanisms responsible were not examined in this study, the patterns of cardiac symptoms identified may help guide future COVID-19 research.
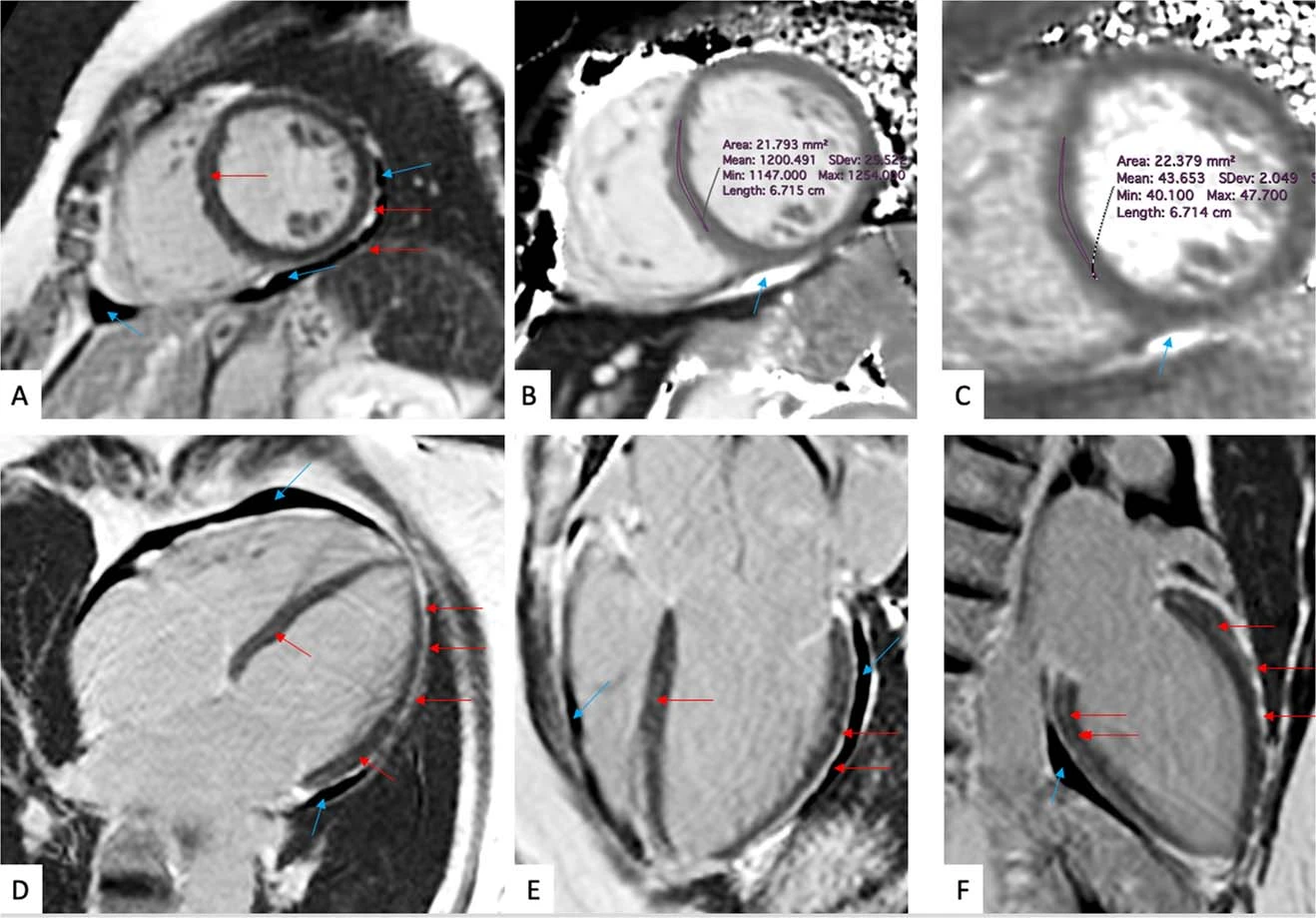
Figure 1: Representative magnetic resonance images of a symptomatic patient evaluated 201 days post-SARS-CoV-2 infection. This individual reported dyspnea, palpitations, and chest pain which worsened upon minimal exertion. © 2022 Puntmann et al., licensed under CC BY 4.0.
Limitations and future perspectives
While this research provides further insight into post-COVID cardiovascular symptoms, the long-term effects of this virus remain unknown. In comparison with the global incidence of the disease, a relatively small number of participants (346 participants, 95 control) were pooled for this study, and replication is required to confirm these findings. Furthermore, while myocardial mapping can provide valuable pathophysiological insights, this technique is not immediately transferable to clinical practice due to a lack of standardization. Nevertheless, these results could prove helpful in characterizing long-term COVID-19 symptoms in the general population, as most studies to date have focused on hospitalized individuals without screening for existing comorbidities or cardiac diagnoses. As we approach the third year of the pandemic, one thing remains clear: there is still much to learn about the effects of long COVID.
About the Author
About the Author

Jasmin Skinner is an undergraduate student at the University of Western Ontario completing a Specialization in Biology and a Minor in Chemistry, with focused interest in applying these concepts to environmental conservation. As a lover of the outdoors and the arts, much of her time is spent in nature and within the local London art community, creating and connecting with all walks of life. After graduating, she hopes to continue her passion of finding unconventional solutions to environmental issues by working with nature, not against it.
References
- Puntmann V, Martin S, Shchendrygina A, Hoffmann J, Madjiguène Ka M, et al. Long-term cardiac pathology in individuals with mild initial COVID-19 illness. Nat Med. 2022 DOI: 10.1038/s41591-022-02000-0. Online ahead of print.
- Huang C, Huang L, Wang Y, Li X, Ren L, et al. 6-month consequences of COVID-19 in patients discharged from hospital: a cohort study. Lancet. 2021;397(10270):220-32. DOI: 10.1016/S0140-6736(20)32656-8.
- Centers for Disease Control and Prevention, COVID-19 [Internet]. COVID data tracker weekly review. 2022 Sep 16 [cited 2022 Sep 14]. Available from: https://www.cdc.gov/coronavirus/2019-ncov/covid-data/covidview/index.html.