Q&A Report: CRISPR-Enhanced Adipocyte Browning: A Cell Therapy Approach to Treat Metabolic Disease
These answers have been provided by:
Michael Czech, PhD
Isadore and Fannie Foxman Professor
Molecular Medicine
University of Massachusetts Medical School
Can you foresee a similar type of treatment being used to reverse diabetes or obesity in humans?
We recognize there are several major hurdles in advancing this technology to the clinic, including scalability to much larger body mass and time frame of viability of adipose implants in humans. Costs must also be considered, and we are encouraged by efforts in other laboratories working in other disease fields to produce “off the shelf” cells that are modified to lower an immune reaction after administration. In order to advance our technology, we are aiming to determine whether we can translate our proof of concept work in mice to larger animals.
Were there any off-target effects of sgRNA used in your study? How did you control them?
Our initial efforts to determine off-target effects by Sanger sequencing around predicted sites of slightly mismatched genomic sequences yielded little evidence of such. We are now embarked on a much deeper analysis of off-target indels and we should have that data soon. One way to minimize such unwanted cleavages by the Cas9 is to test multiple sgRNAs and determine which yields high efficiency of target gene KO with the least off-target effects. There are also modified and new Cas proteins being developed by several labs, with indications that off-target effects may be minimized with such alternative Cas proteins.
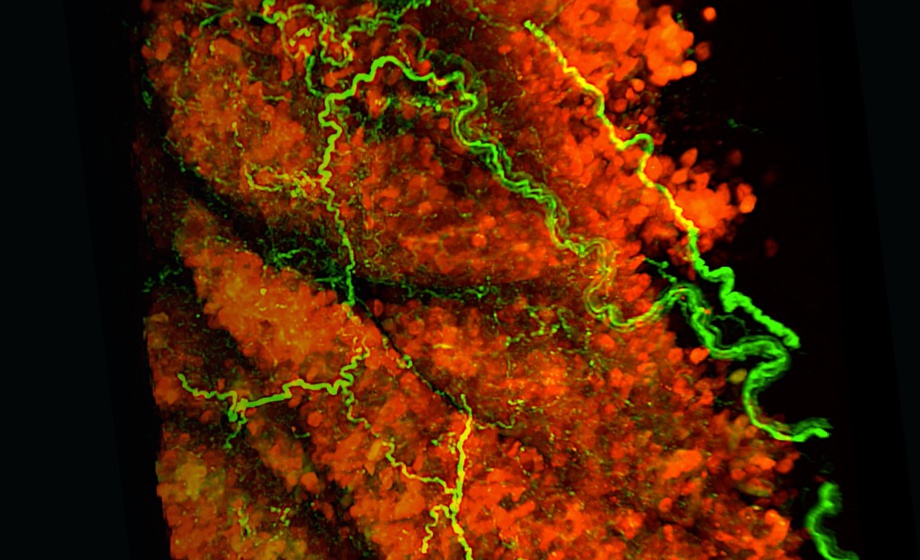
What structural effects in mitochondria could you see?
We were able to easily detect increased expression of electron transport chain components in the Nrip1KO adipocytes as expected from previous work, but we have not performed structural analysis of the mitochondria. Recently, we have also measured oxygen consumption in Nrip1KO adipocytes and determined an increased respiration rate in the presence of norepinephrine compared to control adipocytes treated with Cas9/nontargeting sgRNA. Importantly, oligomycin sensitivity of oxygen consumption was greatly decreased in the Nrip1KO adipocytes, indicating there is a strong uncoupling of electron transport from oxidative phosphorylation due to the expressed UCP1 in these cells. Thus, Nrip1KO does indeed cause increased thermogenesis in adipocytes, along with increased secretion of beneficial factors such as Nrg4.
Would it be feasible to do in situ gene editing of adipocytes, as an alternative to your ex vivo editing and transplantation strategy?
In situ gene editing is a more difficult goal, and our attempts at it so far have not been successful for selectively targeting adipocytes. This would require innovations in cell specificity of targeting as well as in developing stealth Cas9/sgRNA complexes that would not cause immune reactions. Efforts are being made in many labs around the world in such efforts related to a variety of cell types and disease indications, and progress is being made, at least for some tissues such as liver.
What are the advantages of transplanting engineered adipocytes vs targeting endogenous adipocytes?
There are at least a couple advantages of implanting adipocytes that have been manipulated in vitro: First, as shown by the Corvera laboratory, one can greatly expand the number of human progenitors from small samples of adipose tissue, thereby increasing the therapeutic potential due to generating a high abundance of beige adipocytes for implantation. Second, as we show in our BioRxiv paper online, genetic manipulation of the progenitor cells ex vivo can greatly increase the “beige” properties of the human adipocytes generated in vitro, thereby increasing therapeutic potential. If this could be done by safely and specifically targeting endogenous adipocytes in vivo, it would similarly be an excellent approach, but it is not yet feasible.