Q&A Report: Sex, Drugs and Protocol: How Researcher Choices Impact Experimental Outcomes in Preclinical Diabetes Research
I noticed you use the intraperitoneal GTT, not oral gavage, which in fact by using IP injection excludes some hormonal effects. Why not use oral gavage?
We have looked at oral gavage as a comparison to i.p. and voluntary consumption of oral gels and found that it causes higher glucose responses during the GTT than gels, but lower responses than i.p. This is most likely because gavage has similar stress responses to i.p. but stimulates the incretin response like oral gels, as you mention, so it shows the potential welfare benefits of the gels. Overall, I think most labs use IPGTT just out of ease of the procedure and less chance of anything going wrong but we think that the key thing is to understand how the route can alter your results, be aware of that when comparing data to others and be consistent.
How intensive is the surgery? Some in vivo studies are quite large, requiring the use of 50 to 100 animals. Is continuous glucose monitoring practical for these larger studies?
The surgery does require a certain level of technical competence so training would be required (I believe DSI holds training courses). In our hands the surgery takes around 30-45 min. It’s reasonably costly in large numbers so if this is limiting, I would suggest a study in a smaller number of animals can help design a non-telemetry study (or the data resolution may mean you don’t need as many animals). For example, administering a drug to telemetry animals means you can see when the peak response is, which could help you decide at what time point to do glucometer readings in non-telemetry animals.
Have you tried 2- or 4-hr fasts?
Yes, but in between! We did 3 hour fasts. 3h fasts didn’t reduce blood glucose to quite the same extent as 6h fasting, although this wasn’t significant, and 3h vs 6h fasts didn’t alter glucose tolerance during an i.p.GTT. In the end, we decided to focus on 6h fasts mainly because of previous literature showing that at least 4-5h of fasting is needed to ensure hepatic control of glucose concentrations and gastric emptying of food consumed in the dark phase, both of which are the key aims of fasting (see Ayala et al., 2010; Champy et al., 2004; Heijboer et al., 2005; Jensen et al., 2013; Kurokawa et al., 2000). In the future it may be interesting to look at 4h or 5h fasts, but all of this data shows that 6h is sufficient so we focused on that in these studies.
Can isoflurane and oxygen be used to help alleviate the stress generated due to handling? What is the effect of anesthesia for GTT to reduce these variabilities?
We wouldn’t recommend anaesthetizing the mouse as it’s quite well established that also affects the blood glucose concentrations (https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4908499/). Also the act of anaesthetizing is probably as stressful as the IP injection (in males in particular: doing the injection didn’t add on much more stress than the handling itself).
I agree completely that overnight fasting in mice is stressful, but is the DSI glucose sensor actually accurate below 50 mg/dl?
Obviously I can’t say for sure, but we have seen this consistently in different male mice with different sensors. This tends to happen at about 3am on an overnight fast so we have not verified with a glucometer. I have measured mice below 3mM with a normal glucometer and they look surprisingly OK with regard to other behavior, but again perhaps the glucometer was not as accurate at the low blood glucose concentrations. So I think mice can go quite low, but as you infer, it’s quite difficult to be sure how low they actually go. However, I’m very confident that they go much lower than normal and taken together with temperature drops and weight loss I’m pretty sure this is not good for welfare.
When you change the cages for fasting, do the mice stay in the same room, or are they moved to a procedural room? Also, is the GTT being done in the same room as the fasting?
In these experiments the room remained the same for both the fast/cage change and GTT as the telemetry setup is cumbersome so difficult to move and the mice need to be on their receiver mats to acquire the data. However, we have looked at the impact of moving the animals to another room using the telemetry as this is what would be done in a non-telemetry setting. We found that blood glucose concentrations increased by around 40% for up to 60 minutes regardless of whether they were moved into a new room or back into their holding room. This didn’t tend to alter glucose tolerance during an i.p.GTT though, possibly because the blood glucose of mice remaining in the holding room is still increased by all of the other stressors during a GTT like handling, blood sampling and i.p. injection.
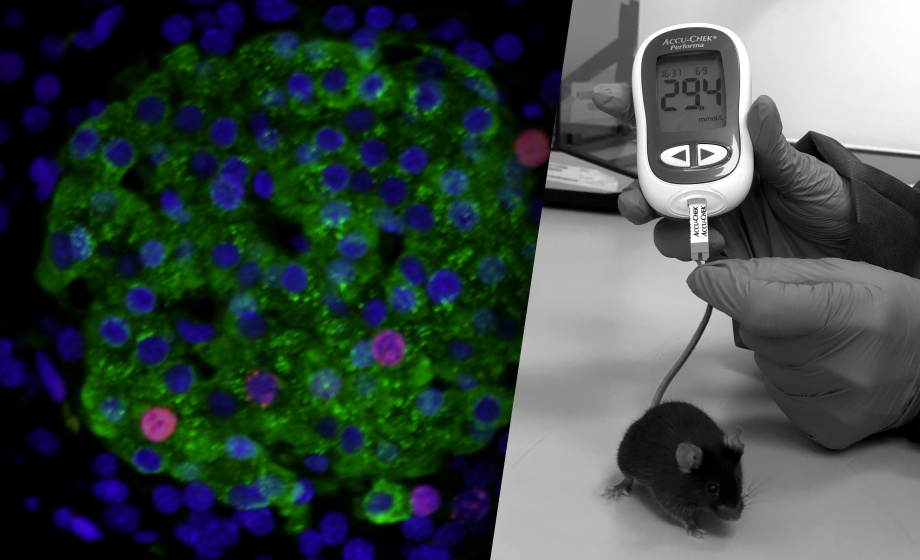
I have seen adverts for mouse-specific glucometers. Does the type of glucometer (human type used in mice) make a difference?
Yes, this study was carried out using a glucometer suitable for mice and they tend to read lower than the human meters (as they account for the different haematocrit levels). However, we have also extensively used human meters in our lab. The key thing is to keep your meter consistent in your study, report what meter you use and be aware of that potential difference if comparing to the literature as exact values may differ. But trends both within and between mice, and within and between experiments should be comparable as long as you are consistent. Also, different meters require different blood volumes, so if more blood is required this could potentially increase the stress response.
There is controversy in literature about glucose injection in GTT based on body weight or lean mass?
This is not an area we have studied in great detail, but we find it doesn’t make a huge difference. This may not be the case if using very obese mice like the ob/ob.
Did you perform a mock GTT to determine whether the differences you observed were do to increased familiarity with the procedure vs a prolonged physiologic response to the administration of the glucose bolus itself?
We did do saline injections to compare the procedure to the effect of the glucose injection. We have also compared the reproducibility of GTTs in the same mice across different time points and after the first time and they were reasonably consistent especially when procedures were more refined (e.g. voluntary gels and 6h vs 16h fasts).
How long of fasting and at what time of the day is it most appropriate to perform glucose measurements?
For our GTT we now fast at 9am and do the GTT at 3pm. We couldn’t find defined times that are “best” to measure non-fasted blood glucose concentrations but we did find that they increase just before the change to “lights off”.
Have you had the opportunity yet to apply the glucose telemetry to older mice, e.g. around 18-24 months, and if so have you noticed any differences in advanced age? The reverse of the high fat feeding experiments hace you tried caloric restriction of the mice with continuous monitoring?
These would both be really interesting to look at, but we haven’t done these experiments.
Do you have the reference of the chocolate sugar free flavour?
We used Nick’s Stevia chocolate drops, which we bought on the internet.