In this webinar, as the tenth part of the Science of Aging Webinar Series, Dr. Dale Abel discusses mechanisms underlying heart failure in aging and diabetes.
Highlights
- An overview of complications associated with diabetes and aging that contribute to heart failure
- A risk assessment of developing cardiomyopathies associated with aging, obesity, and diabetes
- Dysfunctional glucose metabolism mechanisms and heart failure
- Metabolic profiling to determine cardioprotective treatments for heart failure in patients with diabetes
- Review of how cancer metabolism and cardiomyopathies have parallel dysfunctions
Webinar Summary
Dr. Abel begins this webinar with an overview of complications resulting from diabetes and the comorbidities associated with this disease.
“For many years, the focus has been on the microvascular complications such as retinopathy, nephropathy, and neuropathy, but more importantly it is the macrovascular complications that drive most of the suffering and increase the risk of heart attack and stroke.”
He proceeds to present epidemiological evidence that shows trends in vascular complications from the early 2000s. One study revealed that nearly half of patients hospitalized with heart failure also present with diabetes, which led to Dr. Abel’s investigation of whether whole-body glucose metabolic dysfunction leads to cardiomyopathy and resulting heart failure. The first section of this webinar discusses the intrinsic defects in cardiac muscle that increase the likelihood that cardiac dysfunction will develop in the presence of added stressors such as ischemia or cardiac hypertrophy. He then presents data showing that changes in Troponin T, an integral component of the troponin complex in cardiac and skeletal muscle, are predictive of heart failure and mortality in diabetic patients.
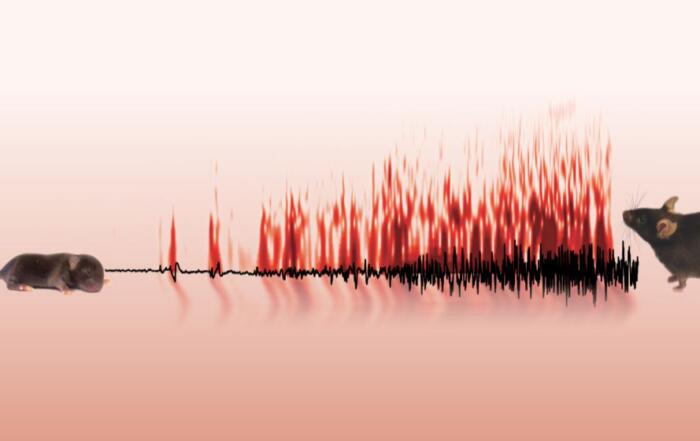
The next part of the webinar focuses on glucose metabolism and specifically outlines “glucotoxicity” and the effect it has on mitochondria. Dr. Abel introduces his group’s work on the effects of dysfunctional glucose metabolism on mitochondrial function. They developed a mouse model in which GLUT4, a glucose transporter in cardiac muscle, is overexpressed. This mutation was sufficient to increase glucose uptake in cardiac muscles and resulted in mitochondrial dysfunction in these mice, including glucose-dependent protein modifications on mitochondrial electron transport chain complexes in cardiac mitochondria. These modifications also change the way that fatty acids are metabolized by cardiomyocytes which leads to further metabolic dysfunction and resulting heart failure.
“Hyperglycemia primes the heart to be susceptible to the consequences of lipotoxicity . . .”
Dr. Abel continues with an overview of the “lessons learned” from metabolomic profiling of patients with heart failure and diabetes to elucidate the mechanisms that can be exploited for treatment and cardioprotection. He highlights work that investigated the mismatch between the rate of glucose oxidation and the rate of metabolite flux through the TCA cycle in patients with left ventricular assistive device (LVAD) implants. They discovered that an increased mismatch between these rates was directly correlated to poorer outcomes in patients with LVAD implantations.
Another study that investigated LVAD implantation outcomes showed that patients with positive outcomes also showed greater glucose metabolic pathway remodelling, which promoted cardioprotection and the resulting recovery from LVAD implantation.
“Heart failure and cancer share a common metabolic soil in the sense that in heart failure, these glycolytic intermediates are really driving the process of ventricular remodelling, while in cancer, these pathways are driving cellular proliferation.”
Finally, Dr. Abel finishes the webinar by presenting studies that outline dysfunction in pyruvate and glucose metabolism and its prevalence in both cancer and heart failure.
Resources
Q&A
- Is it recommended for patients with heart failure to follow a ketogenic diet?
- How does mitochondrial function from the failing hearts in the knockout mice compare with that of wildtype mice, and specifically with isolated mitochondria from cardiac muscle?
- High fat diets promote cardiac hypertrophy, while a ketogenic diet was shown to improve the cardiac phenotype, so is the high fat diet reducing the glucose flux and a ketogenic diet isn’t, or is it a different mechanism?
- What is the role of glucose 6-phosphate at the crossroads of glucose metabolism?
- What is the role of SGLT1 (sodium-glucose cotransporter 1), specifically in the context of diabetes and heart failure?
- Can the same dysfunctions in glucose metabolisms in cardiac muscle be observed in skeletal muscle with the same disorders, such as with sarcopenia, and is there any mechanism that can underlie both cardiac and skeletal muscle changes?
- Are there any stable isotope tracing experiments in these models, and specifically, how do the levels of TCA cycle intermediates change?
- What drives protein degradation in the reverse remodelling?
To retrieve a PDF copy of the presentation, click on the link below the slide player. From this page, click on the “Download” link to retrieve the file.
Presenters
Chair, Department of Internal Medicine; Director, Fraternal Order of Eagles Diabetes Research Center; Professor of Medicine, Biochemistry and Biomedical Engineering
Internal Medicine
The University of Iowa