Dr. Fiona Harrison discusses how dietary deficiency and exposure to toxins can impact glutamate uptake and clearance, and the subsequent changes in neural signaling can be detected through altered EEG activity and performance on learning and memory tasks.
Highlights
- Introduction to the epidemiology and pathology of AD
- Discussion of factors and possible pathological mechanisms contributing to cognitive decline in AD
- Evidence linking epileptiform activity and seizures with cognitive decline and pathology in AD and mouse models
- Studies of electroencephalogram (EEG), long term potentiation (LTP), and memory task performance in wild-type and APP/PSEN1 mice treated with low-dose kainic acid
- Longitudinal studies of immobility, EEG activity, and memory task performance following chronic kainic acid treatment
- Dietary and environmental factors contributing to cognitive decline in AD
- The role of vitamin C in glutamate toxicity
- Studies of behavior, EEG, and glutamate transporter expression in APP/PSEN1 mice following chronic vitamin C depletion
Webinar Summary
Dr. Harrison began this webinar with an introduction to the epidemiology of AD and its defining pathology, including a brief discussion of the recent Aducanumab approval and the beta amyloid hypothesis.
“. . . One of the interesting and in fact really hopeful facets of Alzheimer’s is that there is a huge difference in the clinical manifestation . . . that patients experience in relation to the pathology within the brain.”
Clinical data were presented, illustrating the lack of consistent correlation between amyloid neuropathology and cognitive impairment, however, in contrast, clear associations between amyloid deposition and behavior have been observed in mouse models of AD. This leads to one of the fundamental questions of AD research – how does the underlying basic pathology lead to cognitive decline? A number of possible factors were described, including nutrition, exercise, general health, sleep, education, and environmental toxins. These factors may in turn work via underlying pathological mechanisms such as vascular and metabolic pathways, neuroinflammation, oxidative damage, or neurotransmitter changes.
“To me, the really encouraging thing about Alzheimer’s research is that there is so much we can do in our lives to prevent the cognitive decline, or at least slow its onset, even in the face of pathology.”
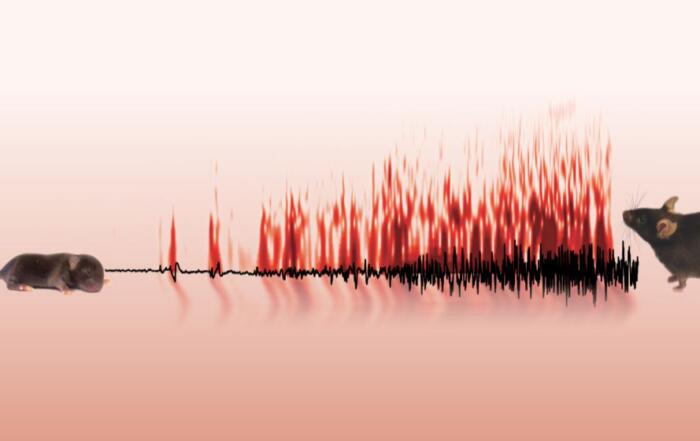
Dr. Harrison’s lab is currently focused on the role of diet and environmental factors on glutamatergic excitotoxicity, and she introduced evidence linking hyperexcitability, epilepsy (including sub-clinical epileptiform activity), and seizures with cognitive decline in AD. Although AD mouse models differ from human disease in many respects, the presence of epileptiform activity and EEG changes may be a particularly useful phenotype as they are found in many of the widely studied models. An experimental protocol was then described, in which wild-type or APP/PSEN1 mice (a mouse model of AD) were repeatedly treated with low doses of kainic acid (an analog of glutamate that induces excitatory postsynaptic potentials) and then assessed for EEG activity and LTP, as well as learning and memory task performance. Initial experiments demonstrated that APP/PSEN1 mice treated with kainic acid exhibited reduced LTP in comparison with other groups, and this was associated with impaired memory retention when performing complex tasks.
“Given these mice were young, otherwise healthy . . . to see anything here . . . at this age after these mild challenges is actually quite exciting to us and indicates just how early in the disease process these kinds of cognitive changes may be occurring.”
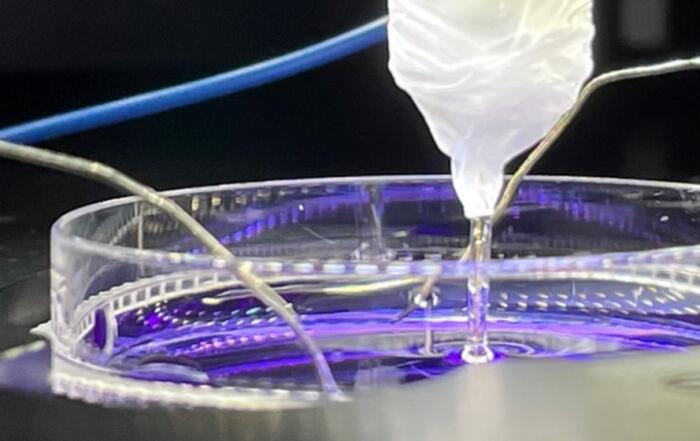
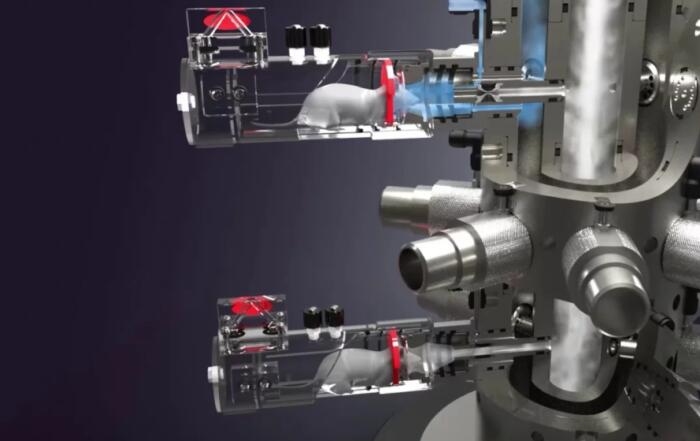
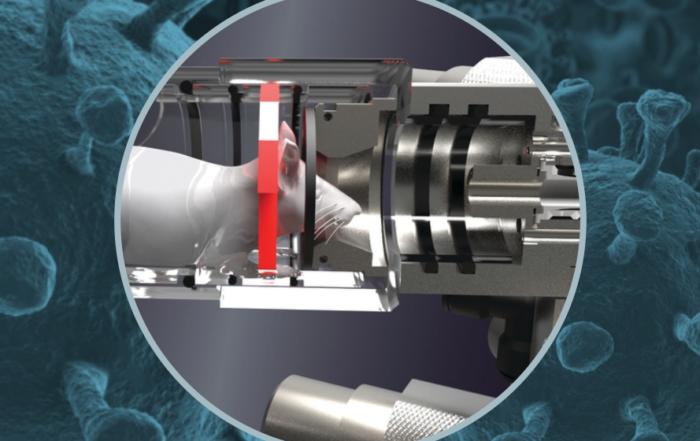
In subsequent experiments, Dr. Harrison’s group used force plate actimeters to detect increased frequency of immobility following kainic acid treatment in APP/PSEN1 mice, and proceeded to study EEG activity over time using untethered DSI telemetry systems. Increases in EEG spikes and spike trains, as detected with Neuroscore software, were evident in APP/PSEN1 mice four weeks after beginning twice weekly kainic acid doses, although these changes were not related to overall changes in sleep patterns.
In the next portion of the webinar, Dr. Harrison discussed potential mechanisms underlying the observed changes in APP/PSEN1 mice following kainic acid administration. Downregulation of EAAT2 (a glutamate transporter, also known as GLT-1) on astrocytes may result in elevated glutamate levels and associated neurotoxicity, and decreased EAAT2 has been observed in postmortem AD tissues. Here, decreased GLT-1 expression was observed following kainic acid treatment and this was further reduced in APP/PSEN1 mice, potentially accounting for some of the observed behavioral and electrophysiological changes reported.
“. . . even very mild perturbations in glutamate signaling can impact cognition and . . . this can be observed through changes in EEG even in very young animals and at very early stages of disease . . .”
Given the potential for glutamate dysfunction to influence cognitive decline, Dr. Harrison discussed a number of putative triggers of glutamatergic systems such as environmental or dietary factors (e.g. manganese, domoic acid, and BMAA), repeated mild traumatic brain injury, and acute illness; one additional important dietary factor is ascorbic acid or Vitamin C, an antioxidant involved in glutamate clearance from the synaptic cleft. Gulo knockout mice require dietary supplementation of vitamin C, and in subsequent experiments gulo-/- mice demonstrated increased susceptibility to kainic acid induced behavioral changes associated with low brain vitamin C levels. Epileptiform activity was then studied in SVCT2+/- heterozygous knockout mice (in which neuronal vitamin C is decreased by approximately 20-30%), suggesting that vitamin C depletion was also associated with EEG abnormalities. Despite the previous findings, longitudinal studies in Gulo-/- APP/PSEN1 mice did not show persistent increases in EEG spike activity when dietary vitamin C was reduced although expected decreases in GLT-1 were observed.
Dr. Harrison concluded the webinar with a summary of sub-clinical and non-convulsive seizure activity in AD, the potential utility of EEG monitoring as a predictor of future cognitive decline, the role of dietary and environmental factors in AD susceptibility and progression, and the potential for early neuropathological changes to better inform future treatment and intervention options.
To learn more about the other webinar in this 2-part mini-series, click here.
Resources
Q&A
- Given the possible direct link between abnormal epileptiform activity and memory impairments are there any behaviors that are likely to be particularly sensitive to seizure phenotypes or kainic acid if tested experimentally?
- Would you expect different EEG results if testing was done during the dark phase?
- Was there any indication of kindling that may have caused a decrease in survival?
- What do you think is the most pathophysiologically accurate transgenic mouse model of AD?
- How well absorbed is the dietary vitamin C provided?
- Do your results suggest antiepileptics may be protective against AD?
To retrieve a PDF copy of the presentation, click on the link below the slide player. From this page, click on the “Download” link to retrieve the file.
Presenters
Associate Professor
Medicine
Vanderbilt University Medical Center