In this webinar, Dr. Rohan Jagirdar presented the results of his research on the acute activation of the thalamic reticular nucleus (TRN) to improve sleep quality in a mouse model of Alzheimer’s disease (AD). He also discussed how chronic TRN activation for 30 days improved sleep quality for the duration of treatment and decreased β-amyloid (Aβ) plaque accumulation in these mice.
Highlights
- Evidence of decreased TRN activity and altered sleep in amyloid precursor protein (APP) mice
- The role of sleep and the TRN in Aβ accumulation in AD
- Evidence of sleep fragmentation in APP mice
- Targeted activation of the TRN in APP mice
- Evidence of decreased TRN activity in AD
Webinar Summary
Dr. Jagirdar began this webinar with an introduction to the mechanisms of cognitive impairment in AD, and the putative role of non-hippocampal brain regions such as the TRN in disease progression. APP mice are a widely used preclinical model of AD, and abnormal TRN activity and associated changes in sleep have previously been reported in these animals. The specific role of the TRN in sleep was described, including sleep maintenance and slow wave sleep (SWS); SWS is decreased in AD and poor sleep is predictive of AD risk several years before the onset of symptoms. Neuronal activity is reduced during sleep and Aβ production is activity-dependent, therefore it is possible that impaired sleep results in increased Aβ due to a combination of increased production and decreased clearance. However, the area of the brain responsible for altered sleep in AD has not yet been identified; Dr. Jagirdar hypothesized that the TRN is the region responsible.
“. . . the field hasn’t identified a specific brain region that is responsible for sleep deficit in AD patients . . .”
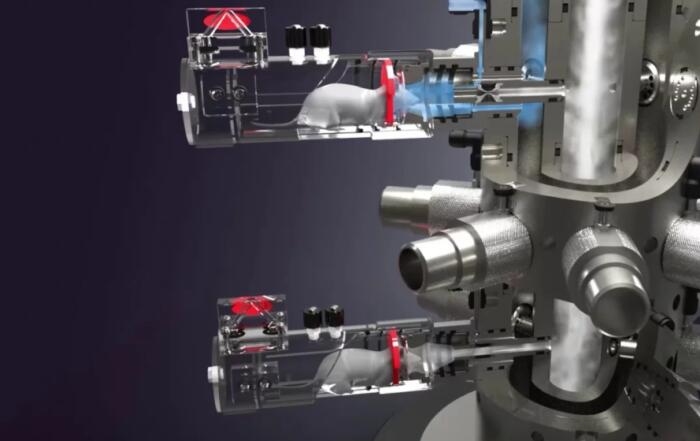
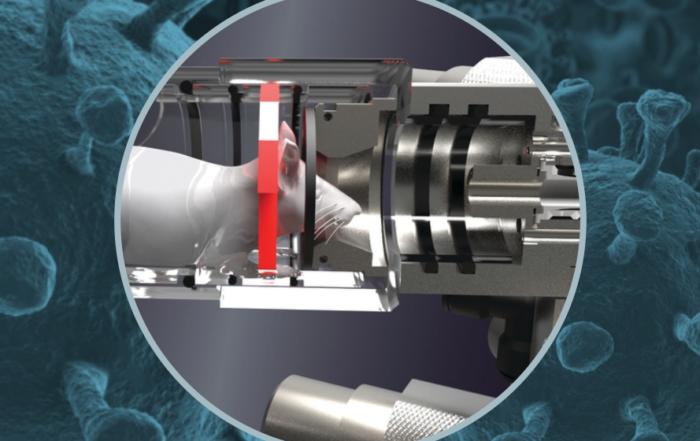
In APP mice, Aβ plaque area in the cortex and hippocampus increased with number of awakenings, and further experiments utilizing DSI telemetry systems to study sleep activity in freely moving mice were presented. Electroencephalography (EEG) and electromyography data revealed increases in time spent awake and decreases in SWS in APP mice as compared to non-transgenic controls.
“We hypothesized that a hypoactive TRN could lead to sleep fragmentation, reduction in slow wave sleep, and that would result in decreased Aβ clearance.”
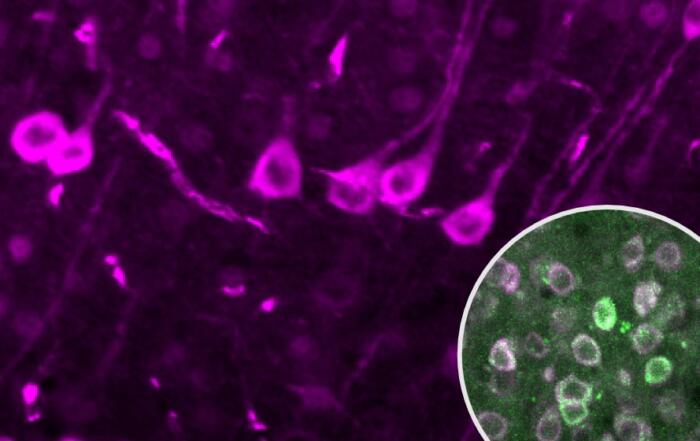
Chemogenetics (also known as designer receptors exclusively activated by designer drugs, or DREADDs) were used to increase TRN activity, in this case by expressing a DREADD in GABAergic neurons in the TRN and selectively activating the receptor with clozapine-n-oxide (CNO). Using this approach, CNO treatment was shown to restore normal SWS and decrease bouts of waking in APP mice as measured by EEG, and in subsequent experiments chronic CNO treatment resulted in reduced Aβ plaque area. Markers of neuronal activity were shown to be decreased in the TRN of postmortem AD samples, and inversely correlated with the severity of AD pathology, despite no evidence of neuronal loss.
“The role of sleep in AD is a really hot topic right now but until now no studies have been able to identify a brain region that is responsible for this sleep deficit, much less find a way to selectively increase slow wave sleep.”
Dr. Jagindar concluded this webinar with a summary of the findings, including increased sleep fragmentation, decreased SWS, and Aβ accumulation associated with decreased TRN activity. However, these effects could be reversed through activation of the TRN, suggesting that targeting this brain region may provide an opportunity to improve symptoms and alter disease progression in AD.
To learn more about the other webinar in this 2-part mini-series, click here.
Click to watch the webinar recording. To view the presentation full screen simply click the square icon located in the bottom-right corner of the video viewer.
Resources
Q&A
- Do APP mice spend more time sleeping in the dark phase?
- Does the TRN show Aβ plaque deposition?
- Were male or female mice used in these studies?
- Did TRN activation reverse cognitive deficits in APP mice?
- Why is TRN activity reduced in APP mice?
- Could the accumulation of Aβ in J20 (APP) mice be responsible for decreased TRN activity?
- In the chronic chemogenetics study were animals dosed daily via injection or continuously via infusion?
- Was there a CNO control group in the chemogenetic studies, and was time of death controlled for in the postmortem AD studies?
- Does oxidative stress affect the TRN?
- Was behavioral analysis performed in these experiments?
- Are there plans to analyze spectral activity during sleep?
- What happens in the TRN if a time shift is induced (jet lag phenomenon), and can TRN activation help with jet lag and narcolepsy?
- Given the absence of any significant changes to REM sleep, is REM normal in APP mice?
- Which neuronal systems, neurotransmitters, and brain regions are involved when the TRN is activated?
- Are there specific biomarkers found in cerebrospinal fluid after TRN activation?
- Were there sex differences in any of the experiments?
- Were there specific awake duration criteria for assessment of sleep fragmentation?
- Does TRN activation have an effect on epileptiform activity?
- Are there differences in sleep spindle parameters after TRN activation?
Presenters
Instructor
Neuroscience
Baylor College of Medicine