In this webinar, Professor Louise Parr-Brownlie highlights the advantages of optogenetic stimulation over deep brain stimulation for treating movement deficits in Parkinson’s disease, while Conor Underwood, PhD, shares tips and tricks for surgically implanting optogenetic devices in rodents.
Highlights
- Overview of deep brain and optogenetic stimulation
- Why a chronically implanted optogenetic stimulation device was needed
- Surgical methods and technical considerations for device implantation
- Tips and tricks for post-operative management
- Reusing telemetry devices
Webinar Summary
Approximately 15% of the population lives with a brain condition that involves death or overactivity of brain cells, such as Parkinson’s disease, dementia, chronic pain, or epilepsy. Another 15% of the population has been diagnosed with a mental health condition such as depression, anxiety, or schizophrenia. Most of these individuals can be treated by behavioral, psychological, or pharmacological therapies; for those who do not respond to these treatments, their intractable symptoms can be treated by surgical interventions. Professor Parr-Brownlie, in particular, is interested in optogenetic stimulation for the treatment of movement deficits in Parkinson’s disease patients.
“Today we’re going to be talking about deep brain stimulation and what might become the next generation of this treatment.”
Deep brain stimulation, approved in 1996 by the Food and Drug Administration, is now used to treat many brain conditions, and the target site depends on the condition and symptoms. In all situations, a frame is attached to the patient’s head, after which the target site is accurately identified by magnetic resonance imaging. During surgery, an electrode is placed into that target structure and a wire is fed underneath the skin to a pacemaker that is located in the chest. Although deep brain stimulation is very effective, approximately 33% of Parkinson’s patients develop side effects such as depression, impulsivity, and cognitive decline.
“Optogenetic stimulation is effective, and that’s the benefit of why we’re developing … this technology.”
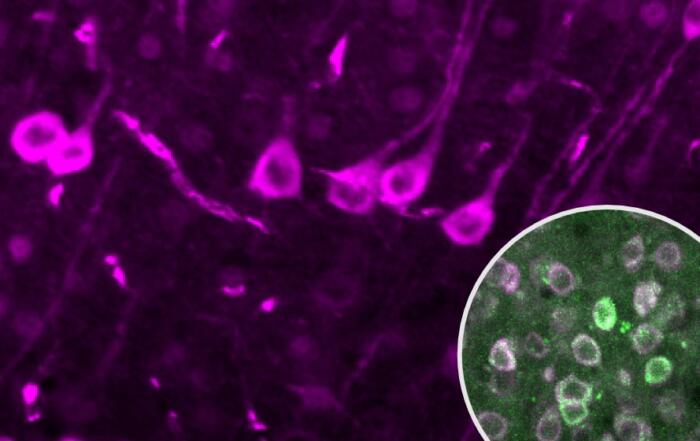
In optogenetic stimulation, only one type of cell, possibly in only one brain region, is actively stimulated, allowing for precise control; an impulse of light activates or modulates the activity of the cell. A virus is injected into the target structure, where opsin is then expressed in the cell membrane. Once expression is robust in target cells, a pulse of light is applied; in Professor Parr-Brownlie’s experiments, blue light is used. An action potential is then created when channelrhodopsin opens.
“The key thing is that with this technology, we can control the flashes of light, and therefore we are trying to recover a function such as movement.”
Professor Parr-Brownlie’s laboratory focuses on the motor pathway for these experiments. Cells within this pathway must be activated at the right time so that a precise movement can occur. In Parkinson’s disease, dopamine cells die off, which are located in the basal ganglia; movement deficits occur when the activity changes within and between these structures. Professor Parr-Brownlie wanted to target stimulation therapy in the motor thalamus; stimulating these cells tends to increase neuron excitability in the motor cortex without directly activating them.
Typically, very high frequencies (i.e., 130 Hz) are used in deep brain stimulation. In one study, Professor Parr-Brownlie’s group investigated whether more complex patterns like theta burst stimulation or reaching patterns could recover motor function more effectively. The results from this study indicated that complex stimulation patterns in the motor thalamus improved movement deficits in a rat model of Parkinson’s disease, while 130 Hz standard stimulation did not; a video example of these experiments is also provided.
“So now that we’ve found that motor thalamus stimulation can recover function, we were starting to think about how we might actually use that or apply that knowledge.”
Important considerations for translating this work to humans is that the human brain is significantly larger than the rat brain, so the technology must be changed to allow for stimulation of a larger brain area. Additionally, Professor Parr-Brownlie did not have an appropriate device when beginning this translational research. For deep brain stimulation, the device is typically implanted in the patient for more than five years at a time, and stimulation is applied continuously throughout the day to treat movement deficits. Therefore, an implantable optogenetic device that could apply complex stimulation patterns was needed, as well as a system to recharge the battery for long stimulation periods. The group collaborated with bioengineers who had developed this device, and fed information back to them so that the device could be refined to a usable product.
In the second portion of this webinar, Professor Parr-Brownlie’s post-doctoral fellow, Dr. Underwood, highlights surgical procedure methods and technical considerations for this type of work. Important aspects to consider include what drugs will be required, rat weights and strains, and what specialist equipment is needed. When preparing for the surgery, Dr. Underwood recommends attaching a cannula to the end of the optical fiber so that the fiber can be guided to the brain without being damaged. Dr. Underwood also recommends coiling the optical fiber and tying excess material off since a long fiber can accumulate in the abdomens of the animals and tangle with the gastrointestinal tract. Additionally, one should familiarize themselves with the optical fiber’s physical properties to know how much it can be bent before it snaps.
“I’m going to show some videos and images of various points in the surgery that are quite unique to this device.”
Dr. Underwood next provides videos to illustrate the typical incision size, how cables are tunneled to the brain, how the steel rod is inserted, how the animal is placed in the stereotaxic frame, and optical fiber bending. Photos are also shown to illustrate the process of building the dental cement headpiece to protect the cables in the head, as well as the final product; there should be enough dental cement to cover the biopotential cables and optical fiber, but not so much that it impairs the animal’s behavior. Lastly, Dr. Underwood recommends closing the abdominal wound with a buried intradermal continuous suture rather than surgical clips to avoid potential infections.
Various measures can be taken to enable post-surgical recovery. The animal’s home cage should be modified to accommodate the headpiece; additionally, warped cages with concave floors can impair device charging. Hard bedding (i.e., corn or wood) should be replaced with paper or cotton to avoid pica behavior by the rodent. Pain and infection should be tackled prophylactically for three days post-operation, or longer if seroma develops. Lastly, Dr. Underwood recommends looking for exposed wires and optical fiber at the rear of the animal’s head, as well as repairing any abdominal wounds immediately to avoid infection.
To conclude this webinar, Dr. Underwood highlights that the telemetry device can be explanted and reused, depending on how much optical fiber must be trimmed. The easiest and least time consuming method of explanting the telemeter involves cutting the cables and fiber closest to the headpiece rather than removing the entire headpiece. Scalpel blades are recommended over scissors when possible to avoid cutting cables in subcutaneous and peritoneal spaces.
Resources
Q&A
- Why is the open configuration for the stereotaxic frame better for implantation?
- Do you need transgenic animals for this type of work?
- How long do you wait after making the headpiece before closing the abdomen?
- How are you closing the skin surrounding the dental cement?
- How stable is the telemeter while the rat is moving?
- What is the longevity of the biopotential implant?
- Can we use ketamine-xylazine instead of gas anesthesia for this procedure?
- Where do you see the future of this technique?
Presenters
Associate Professor
Anatomy
University of Otago
Post-Doctoral Fellow
Anatomy
University of Otago