Q&A Report: Multimodal Neuroimaging Using Functional Ultrasound (fUS)
These answers were provided by:
Davide Boido, PhD
Tenured Researcher
NeuroSpin
CEA – Université Paris Saclay
Antoine Bergel, PhD
Postdoctoral Fellow
The Neuro, Montreal Neurological Institute
McGill University
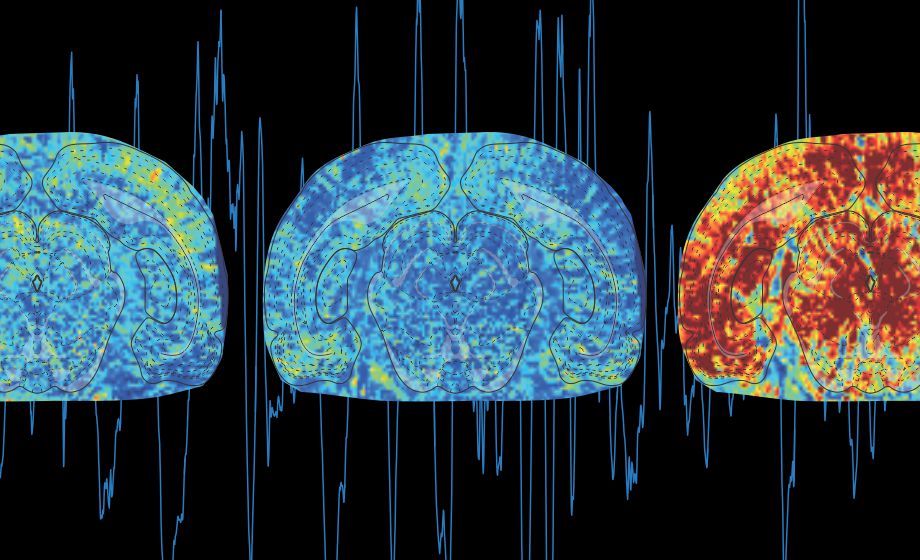
Does the ultrasound scanner create artifact in the electrophysiological signals? Can fUS imaging modulate brain activity locally?
Antoine: Though we cannot exclude interactions between ultrasound (US) waves and brain tissue, we are confident that they do not create noticeable artifacts in the electrophysiological (ephys) signals provided proper grounding (ultrasonic pulses are clearly visible on the ephys recordings when the animal is not properly grounded). Second, ephys traces are identical when the ultrasound probe is close or far from electrodes or even when the scanner is off. Last, though it is known that US signals can modulate brain activity locally, it is mainly the case with focused waves. This is less of a concern here, as we are using plane waves, though it requires keeping the emission voltage and pulse repetition frequency low.
Is it possible to use standard silicon probes (Cambridge Neurotech, Buzsaki probes, Neuropixels) in combination with functional ultrasound?
Antoine: Absolutely. All that is demonstrated here with bundled wires for local field potential (LFP) recordings is transferable to silicon-probes. The only issue would be to implant them without hindering the field of view.
What is the biggest obstacle to safeguard the implant’s integrity for extended periods of time (weeks, months)?
Antoine: The biggest obstacle is the mechanical stress on the implant resulting from routine shocks in the animal’s cage together with the constraints imposed when repeatedly mounting and dismounting the probe into the holder. A compact design during the surgery and fixation screws help solve these problems.
How can you relate the fast dynamics of electrophysiological events to the slow hemodynamics in your studies?
Antoine: As for multimodal imaging using fMRI or optical techniques, ephys activity can be temporally smoothed to compute cross-correlations over comparable time windows. Another option is to re-align slower activations recorded with fUS to the onset of fast events/trials and compute mean response functions. Importantly, fUS’ high signal-to-noise ratio allows us to visualize transient events and assess the variability of vascular responses across trials.
Why did you say that the choice of the olfactory bulb was unfair for BOLD fMRI?
Davide: BOLD fMRI is particularly sensitive to magnetic field inhomogeneities, and interfaces, for example between tissue and bone or bone and air, produce inhomogeneity. This phenomenon becomes more critical when scaling up with the static magnetic field. Our setup consisted of the mouse olfactory bulb scanned at 17.2T. It means we were willing to look at a tiny structure (2x2mm FOV) surrounded by air. This is, usually, manageable even at 17.2T, but the presence of a plastic cover on the top of the olfactory bulbs, although fMRI-compatible, broke the continuity of the tissue-to-bone interface, making it very hard to get fMRI data and imposing some limitations, like a slow TR.
Previous papers, for example on fMRI, showed that the relationship between the stimulus strength and the BOLD response is highly non-linear. Instead, you found a linear relationship: can you comment on that?
Davide: This is because, in most cases, when assessing the linearity of the BOLD responses, the question does not refer to the neurovascular coupling, i.e. the relationship between neuronal and blood vessels activation, but to the stimulus to BOLD responses. Working in humans, for example, does not allow collecting information on neuronal and BOD activation easily. In our case, we had a complete dataset of the same mice: neuronal, microscopic/mesoscopic vascular activation, and BOLD fMRI and we could refer everything to the neuronal activation. The impact of our work to human recordings is that the source of the measured non-linearity is probably completely due to the way neurons encode the stimuli, while the actual neurovascular coupling is linear.
Would you care to speculate about the relationship between hemodynamics and gamma? You mentioned that gamma could be causal, but how would one test that? Lastly, theta also couples with hemodynamics but is less dynamic?
Antoine: The causality still needs to be demonstrated. What we have shown is that gamma activity precedes vascular events by 1.5 to 2 seconds and that fast gamma (80-120 Hz) amplitude is correlated with the amplitude of the subsequent vascular surge. Theta (8-12 Hz) does also correlate but less significantly (see Bergel et al. 2018).
Is it possible to obtain resolution at the level of blood vessels in the choroid plexus?
Antoine: This would depend on the vessels’ size, blood flow, amplitude, and orientation in the choroid plexus. Because we are able to resolve much smaller structures, I reckon this is feasible in the case of the choroid plexus too.
Can these experiments be performed in behaving mice?
Antoine: Yes, but current ultrasound probes remain heavy for behavioral assays – in freely-moving mice together with the stiffness of the cable that can be an issue. Such parameters are constantly improving though.
Which parameter do you use to remove the movement artifacts during running? Do you substract the signal outside of the brain?
Antoine: The only preprocessing step here is to normalize pixel activity by a baseline signal (similar to ΔF/F in optical recordings). Such baseline can either be extracted live at the beginning of the recording or offline during analysis (like re-referencing in electrophysiology).
How does craniotomy affect the intrinsic brain activities? Is it possible some unexpected changes in the brain activities could be attributed to craniotomy induced inflammation?
Davide: Of course, craniotomy is not neutral to brain activity or physiology. One of the most important aspects is the temperature drop induced by the lack of bone, skin, fur etc.. We published a paper on the consequences of temperature on (superficial) brain activation in terms of neuronal, blood flow, and oxygen measurements (Roche M et al., eLife, 2019; doi.org/10.7554/eLife.47324). Inflammation is also a potential issue. However, if the surgery is performed in clean conditions and we allocate enough time to the mice to recover from the surgery (at least 1 or 2 weeks), the inflammation is usually very low or absent (confirmed by immunostaining post mortem). The advantage of placing transparent windows is also to check for inflammation already by the naked eye; the dura mater is red or opaque during an inflammatory state. Regarding the long-term impact of these chronic cranial windows on the animals’ health, I did not notice any particular change in animals’ behavior in the cage, nor a shortened life expectation. I could image the very same mouse from 2-months up to 24-month age with Two-Photon and fUS.
Can we combine the fUS with miniscope and optogenetic stimulation approaches?
Davide: Regarding optogenetics, we did it already in 2017, see: Rungta et al., Nature Communications, 2017: doi.org/10.1038/ncomms14191. Pay attention to the direct effect of light on the blood vessels!
Antoine: About miniscopes: absolutely. The place needed on the animal’s head might be an issue, depending on the model used.
What can we expect from translational development to apply fUS to scalp intact humans?
Davide: Efforts are ongoing in this direction, mainly to exploit the compensation of acoustic aberration made by the bone developed for focused-US. Another option that has already been published in a peer-reviewed paper is to pass-through the temporal bone, see: Demené et al., Nature BiomedEng, 2021: doi.org/10.1038/s41551-021-00697-x.
Is the resolution of this imaging high enough to be able to measure deficits in mouse models of neurodegenerative disease such as stroke, traumatic brain injury, or Alzheimer's disease?
Davide: The question should be more about sensitivity, than resolution. FUS has a very high spatial and temporal resolution. In addition, it also has a high sensitivity to (fast) changes in cerebral blood volume. Because of the novelty of the technique, papers of fUS to study pathology are only a few, but I do not see any specific limitation of fUS to tackling pathophysiological questions.
How does temporal resolution of fUS relate/compare to fMRI?
Davide: Both BOLD fMRI, particularly at ultra-high magnetic field, and fUS can catch the dynamics of vascular changes, such as functional hyperemia, that is relatively slow. Even if I showed that the neurovascular coupling occurs in some hundreds of milliseconds (and not in seconds as it is commonly believed!), BOLD and fUS Power Doppler allows temporal resolution in the range of 200-300 msec. FUS can even go faster, up to a few ms, but, usually, this is not necessary for the vast majority of studies and the fast sampling comes with quite some noise to deal with.
Can you provide details for modelling?
Davide: Is modeling referring to Transfer Functions? If this is the question, all the details could be found in Aydin et al., Nature Communications 2020 (see also supplementary material) doi.org/10.1038/s41467-020-16774-9 and in Aydin et al., PLOS Comp Biology, 2021, doi.org/10.1371/journal.pcbi.1008614.
Can recording ephys disrupt the fUS measurements (ie electrodes damage tissue) or vice-versa?
Antoine: See the previous answer for the effects of fUS on ephys. Implanting electrodes is invasive but it is possible to use thin wires to minimize tissue damage without affecting the vascular structures (though acute bleeding can be observed during implantation) and the resulting fUS images.
Is a craniotomy necessary?
Davide: No but it helps a lot, particularly working with rats and looking at the deep/ventral brain regions, like the thalamus, having a craniotomy significantly improves the SNR.
Antoine: Another alternative is to inject contrast agents like microbubbles in the circulation (see Maresca et al. 2020).
What are the current limitations of fUS?
Davide: It can be used in humans only in particular conditions: babies or through the temporal bone. The sensitivity to RBCs is not isotropic, but it is maximal in the direction of the probe. For functional analysis, there is only commercial SW available and not (yet) open source pipelines, like for fMRI.
Any information on functional ultrasound mapping in macaque monkeys would be appreciated!
Davide: See: Blaize et al., PNAS, 2020; doi/10.1073/pnas.1916787117.
Antoine: See Dizeux et al Nat Communications 2019.
How does fUS compare to fMRI or PET in terms of cost, causality vs. correlation, as well as spatial and temporal resolution?
Davide: FUS is functional CBV at high spatio-temporal resolution and high sensitivity. It does not apply to humans, apart from specific conditions. The average cost of a fUS machine is roughly one-tenth of a MR or PET-scanner and the fUS machine is on wheels, and it can be moved easily. FMRI is mainly BOLD, also dependent on blood flow and it achieves similar spatio-temporal resolution but a lower sensitivity to oxygen transients. However, fMRI can exploit other contrasts, such as diffusion. MRI and PET also allow the monitoring of specific molecules inside the brain. In addition, with MRI you get the brain anatomy, while fUS only shows the blood vessels. However, co-registration approaches exist to deduce the brain location from the vasculature maps.
Causality vs correlation: fUS indirectly ‘counts’ the RBC in a voxel at a given time via the Power Doppler effect. FMRI methods indirectly deduce the neuronal activity via the vascular activation or from other physical phenomena, like cell swelling, the hypothesis at the basis of diffusion-weighted fMRI.
What are the pros and cons of applying this method when compared to others more commonly used for in vivo experiments in mice?
Davide: It strongly depends on the experimental needs and the availability of instruments, like a MR scanner. Now, fUS is limited to a single brain section, while with fMRI we can scan several sections ‘simultaneously’.
Antoine: Significant information can be extracted from the temporal resolution of fUS and its portability which allows its use in a wide range of contexts and models.
Could we incorporate fUS to locate brain regions/structures, so that we can confirm the insertion of electrodes, in the desired structure, during electrophysiological studies in the brain?
Antoine: Yes, absolutely, but the electrodes would need to be moving though so this could be possible during implantation. If fixed, they can be imaged with standard Bmode imaging available on the fUS scanner.
Can this technology be used to identify the cause of OCHOS Syndrome?
Davide: FUS provides functional CBV, so, if the pathology could be modeled in animal models compatible with fUS and the drop in CBF also implies a decrease in CBV, in principle, fUS should catch it. About the cause….Good work!
What are the challenges of coupling fUS with EEG?
Antoine: This is discussed in detail in the second talk: 3 main challenges (1) designing long-lasting implants (2) not impeding behavior (3) multimodal data analysis.
What are some other alternative relevant and easily interpretative techniques other than fMRI for neuroimaging?
Davide: If we refer to studies on animal models compatible with fUS, other than fMRI, but with a mesoscopic field of view, there are the laser Doppler or the intrinsic optical signal approaches, although with limited tissue penetration. Alternatively, there is optoacoustic tomography, that has been recently compared to fUS, see Robin et al., NeuroImage, 2021; doi.org/10.1016/j.neuroimage.2021.118111.