Q&A Report: Spatiotemporal Dynamics of Calcium and Neurotransmitters in Awake Mouse Models of Epilepsy
The answers to these questions have been provided by:
Vincent Magloire, PhD
Wellcome Senior Research Fellow
Department of Clinical and Experimental Epilepsy
Institute of Neurology, University College London
Ken Berglund, PhD
Assistant Professor of Neurosurgery
School of Medicine
Emory University
Could the longer decay in GABAsnfr be simply due to differences between the kinetics of GABA and GLUsnfr indicators?
VM: It is a good point. iGluSnFR and iGABASnFR have relatively similar intrinsic off-rate kinetics, at least when measured in in vitro preparation with a single electrical stimulation. See Marvin et al., 2013, 2019 Nat. Methods.
How many CSDs (cortical spreading depolarizations) have you recorded in the PTZ model? Just one CSD or more?
KB: While not every PTZ-induced seizure was followed by a CSD, when one did follow, it was a single CSD per seizure. CSD has a relatively long refractory period (tens of minutes), and we did not attempt to elicit more than one seizure per recording session. This also helped us to prevent kindling effects of PTZ and to decrease mortality. However, CSD can be reproduced in the same animal in another imaging session on another day.
Maybe to both of you, can you exclude signal contributions due to hemodynamic changes? Or did you control for that in any way?
VM: We cannot completely exclude the contribution of hemodynamic signal. However, in a subset of experiments, we used 2 control SnFR variants. 1. We used an insensitive iGABASnFR for GABA. In this case, we cannot see much signal variation correlated with IIS and seizures (See Supp Figure 7, Shimoda et al., 2023 Brain). 2. We also used another iGABASnFR variant (sensitive to GABA) linked to mRuby tag (red fluorophore insensitive to GABA) on the intracellular side. Same as the first control, the ratio iGABASnFR/Red signal suggests very little contribution of the red channel to the overall signal during epileptic activity (in our settings: spiral scan, very superficial imaging, small area, etc..).
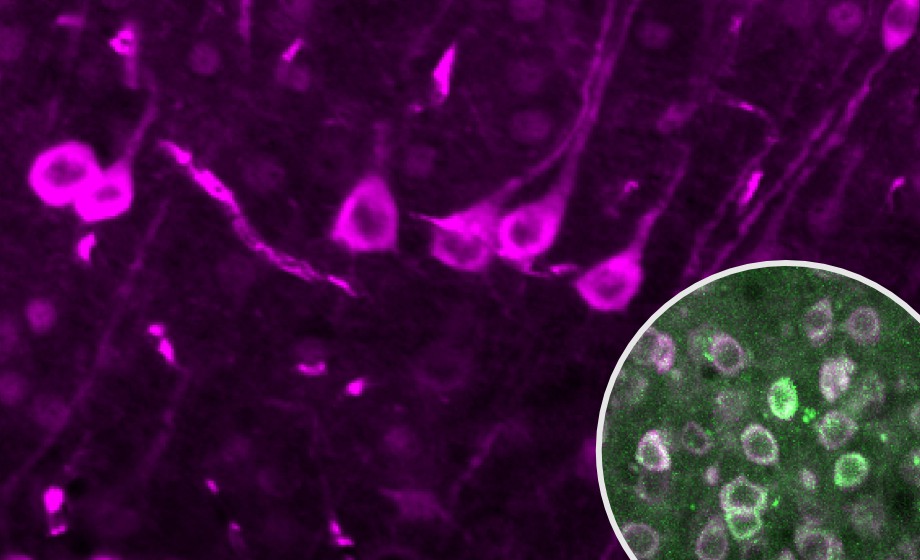
KB: We do not have a specific control for hemodynamics, yet the nature of our methods and processing should ensure negligible contamination. Classically hemodynamic contributions are concerns for 1-photon imaging, particularly widefield, where there is more out of plane excitation and light scattering. The nature of 2-photon laser scanning intrinsically avoids much of the hemodynamic contamination, with optical sectioning with narrow point spread functions. Additionally, we are looking at only somatic transients and, with our processing, we are subtracting a percentage of signal from the surrounding neuropil, further refining our signal. Furthermore, we exclude any regions that overlap with major blood vessels from our analysis.
In which anatomical direction do CSDs propagate? Is it away from the seizure focus, as Dr. Magloire showed with his GABA imaging?
KB: While we have observed CSDs propagating in all directions across our experiments, we find they predominantly propagate anteromedially. We believe this is consistent with our model (systemic injection of PTZ) of generalized seizures which don’t have a distinct seizure focus in the neocortex.
I have a question for Ken Berglund: Can we record the Ca2+ current during a spontaneous seizure (e.g. chronic phase)?
KB: For this you need a model with low mortality, but a high seizure frequency, of which there are very few, and even those tend to be rather inconsistent across animals. These models also tend to be electrographic only; behavioral and/or generalizing seizures occur a few times a day at best. With that one would need to record for several hours with the hope that one is collected. Some other practical obstacles are the huge amount of data collected and well-being of the animal under long-term head fixation. There is also the risk for photobleaching of your indicators with prolonged imaging. For these reasons, we only image for up to 1 hour a day per animal. Perhaps, a reliable seizure prediction algorithm could circumvent much of these problems.
To Dr. Berglund: Regarding the spread of Ca2+, is the spread via synaptic transmission or via gap junctions? If it is via gap junctions, which type? Similar question to your ER-Ca signaling depression-spread.
KB: Spread of Ca2+ among neurons during a seizure is mediated by synaptic transmission as Vincent’s and other people’s studies have shown. There have been studies looking into astrocytes, which form large gap junction networks, showing Ca2+ flow through them during seizures. For CSD there have been several studies looking at gap junction mediated transmission, which predominantly reject their necessity. However, there have been a few studies showing the opposite and, thus, it is still an open question in the field. While we postulate that neuronal gap junction does not play a significant role in CSD, we nevertheless would like to apply a gap junction blocker to see if this impacts the Ca2+ dynamics we observe. Another possibility we are considering is the flow of IP3 through gap junctions, which could contribute to CICR.
To Vincent: Based on your data, do you think interictal bursts are a spatially contained irregular electrical activity that can "escape" into ictal activity, or do you think ictal activity has a completely different mechanism from interictal bursts? If the former, what would you say is the mechanism for the "escape"?
VM: According to our data, it is the first option, but it is in acute models of epilepsy, and it is important to keep this in mind. Interictal and sentinel spikes (seizure onset) cannot be distinguished electrographically or while using calcium imaging (see Rossi et al. 2017 Nat. Comm). However, using iGABASnFR and iGluSnFR imaging, we clearly see a decrease in amplitude of the GABA transients accompanied by an increase of glutamate signal at seizure onset when compared to IIS. This suggests that overexcitation escapes the local inhibitory restraint. This escape can be explained by a presynaptic decreasing of GABA release involving one (or more) of the 3 following mechanisms:
1. Vesicle depletion,
2. pre-synaptic inhibition by GABAb receptor activation,
3. a proportion of local interneurons enter a depolarization block state.
In Shimoda et al., 2023, we tested whether inhibitory population undergoing fatigue alone in a simple mean field model could reproduce our main experimental findings, which it did. In addition, although all 3 mechanisms are not mutually exclusive, the first two would require repeated spiking activity above 10 Hz which is not the case in our models (IIS frequency ~ 0.02-0.5Hz). So, the 3rd mechanism is the most probable but remains to be further investigated in vivo.
How do you think the 3D in vitro models will help in this area?
KB: The whole animal is a better model to study epilepsy for sure, but it is also true that the genetic imaging method we employed cannot be used in humans, except for brain organoids. We might be able to gain invaluable insights if we use brain organoids derived from epilepsy patients.
How high does intracell Na+ peak during seizure or SD and are there accurate intracellular dyes to answer that?
KB: While we do not specifically look at sodium here, I will point you to Jens Dreier’s 2015 review in Neuron which has a helpful table of ion concentrations: Intracellular Na+ is 16 mM during seizure and 35 mM during CSD. In terms of imaging, there are organic fluorescent dyes for Na+, but we are not aware of its usage in vivo. Loading and retention are always an issue when a synthetic dye is used in tissue. We could potentially use reversal potential of sodium conductance, but in vivo patch clamp is an extraordinary technique.
How best to optimize parameters in two-photon calcium imaging?
KB: We try to avoid two things: photobleaching of the indicators and saturation of the detectors. The former is a relatively minor issue because of the usage of two-photon microscopy and genetic indicators: Only a fraction of the indicators is excited inside a cell in a small focal volume and they are replenished inside the cell as they diffuse through the cytosol (membrane bound indicators tend to photobleach faster). Saturation is a unique problem with seizure physiology as the calcium increase can be huge during a seizure. We titrate the gain and laser power so that we will not experience saturation of the PMTs, but even so it is difficult to examine firing dynamics during an ictal event with the slow decay constants of calcium indicators.
Do you have any evidence that depletion of ER calcium is indeed mediated by calcium-induced calcium release?
KB: We do not yet have definite evidence, although the time course suggest that it is the case. We would like to conduct pharmacological experiments to answer this question more directly.
Does the red ER calcium sensor show photoswitching behavior? Can it be combined with other green fluorescent proteins and optogenetics?
KB: We did not observe any photoswitching of R-CatchER when excited by the two-photon laser. This doesn’t mean that it does not show photoswitching even with wide-field excitation. In fact, mApple, which the ER indicator is based off, is known to show photoswitching. Even if the fluorescent indicator photoswitches, it is not an issue for our experiments as we only use a single wavelength to excite the two indicator proteins with overlapping excitation spectra.
Is spreading depolarization actually anti-epileptic? Is there any downside?
KB: Our observations are consistent with the evidence in the literature that CSDs likely have a seizure-suppressive effect. While it is potentially enticing to consider inducing CSDs as an anti-seizure treatment approach, these are pathologic events nevertheless that bring neurons to near death. CSDs have serious implications and risks. In the face of the widespread aberrant activity of a seizure, essentially turning off a neuron with a CSD is likely the lesser of two evils, but that is only if the neuron recovers, which in a normoxic state is more likely than an anoxic state. Thus, we feel, further dissection of the anti-seizure suppressive mechanism of CSD is needed if it is to be leveraged toward treatment development.