CBD’s Potential as an Anti-Cancer Agent
Blog post by Jasmin Skinner
Chemotherapy is one of the most effective cancer treatments available today, but the side effects can be extremely difficult for patients to tolerate. These effects may be short- or long-term, and may include hair loss, low blood cell counts, changes in taste and smell, memory and cognitive impairment, changes in vision and hearing abilities, as well as organ damage (1). Chemotherapy agents are designed to target the fastest actively dividing cells, which, while very effective at preventing cancer cells from growing and dividing, can also subsequently affect normal dividing cells, such as blood cells within bone marrow, or hair follicle cells (1).
Despite significant advances in chemotherapy, radiation therapy, and surgical options, cancer remains the second leading cause of death in the United States. Explore the use of vaccines for the prevention and treatment of cancer in this blog, and learn about a number of existing therapies and the potential clinical use of cancer vaccines. READ HERE
Certain chemotherapy drugs, like cisplatin, are so effective at targeting cancer cells that they’re used against several different types of cancer, including carcinomas, germ cell tumors, lymphomas, and sarcomas (2). However, due to numerous side effects like drug resistance and severe kidney damage, this chemotherapeutic is often used in combination with other anticancer drugs to reduce toxicity and the likelihood of drug resistance (2). While this approach is more effective at targeting drug-resistant cancers, patients who receive a mix of chemotherapy drugs often experience more severe and prolonged side effects than individuals who receive a single drug, further exacerbating this problem and potentially worsening a patient’s quality of life (3). The challenge facing clinicians and researchers is therefore to identify and apply effective anticancer therapies while simultaneously limiting the severity and prevalence of side effects.
Cannabidiol (CBD) is one of many active ingredients in cannabis, with potential therapeutic applications including treatment of anxiety, insomnia, and chronic pain (4). In addition, CBD has also shown potential as an antitumorigenic agent capable of attenuating the severity of certain adverse side effects of chemotherapy. Two recent studies have sought to determine the effects of CBD in cancer patients receiving chemotherapy; specifically how CBD can help treat cisplatin-resistant non-small cell lung cancer, and also how it may reduce kidney damage from cisplatin treatment (5,6). In this blog, we discuss the antitumorigenic and anti-inflammatory effects of CBD, and also discuss additional considerations and limitations of CBD use for patients receiving chemotherapy.
Treating cisplatin-resistant non-small cell lung cancer with CBD
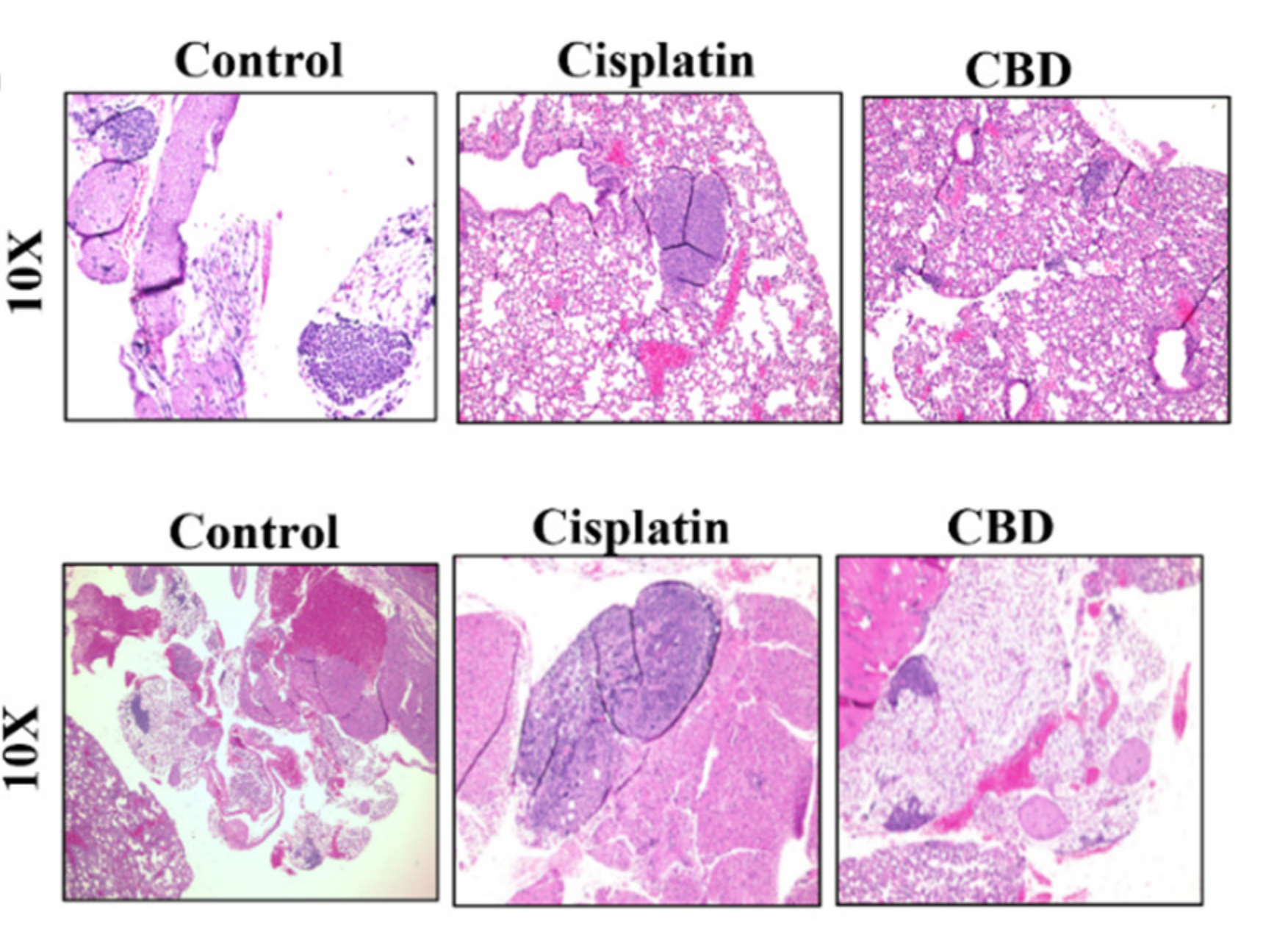
Non-small cell lung cancer (NSCLC) has been used to model cisplatin-resistant cancer; as tumor removal is often precluded due to structure and location, cisplatin chemotherapy is the primary method of treatment for this disease. While this method is effective at the start of treatment, drug resistance ultimately develops, potentially resulting in tumor recurrence. This pattern of resistance and recurrence is often attributed to the development of cancer stem cells, which are self-renewing and capable of escaping the cytotoxic effects of chemotherapeutic drugs such as cisplatin. Based on recent studies demonstrating that CBD oil improved tumor regression in lung adenocarcinoma patients in the absence of chemotherapy, Misri et al. sought to determine whether CBD could be an effective inhibitor of cisplatin-resistant (CR) NSCLC compared to cisplatin treatment alone. To do this, large cell carcinoma cells and adenocarcinoma cells were obtained and made cisplatin resistant, and then cultured and suspended to form cancer stem cell spheres. These cultures were treated with a vehicle control, CBD, or cisplatin and then analyzed to determine the percentage of cancer cell apoptosis. Additionally, the same treatments were applied and evaluated in a mouse model of CR NSLSC to further validate these findings (5).
Anti-tumorigenic effects of CBD
CBD was observed to not only induce apoptosis of cisplatin resistant non-small cell lung cancer cells, but also reduced their viability, and inhibited sphere formation and stemness gene expression. As cancer stem cell spheres play a key role in drug resistance development, the effectiveness of CBD in reducing these populations within cisplatin-resistant cell lines demonstrates promise for chemotherapy-resistant cancers. Additionally, while CBD is derived from cannabis, no psychoactive or other adverse effects were observed, demonstrating the relative safety of this treatment in isolation (5).
CBD induced apoptosis in these cisplatin-resistant NSCLC cell models via the TRPV2 ion channel. Recent studies have shown that CBD is able to directly interact with this channel, and that it is more highly expressed in lung adenocarcinoma than other cancer types. The findings from this study suggest that TRPV2 could be used as a diagnostic biomarker for NSCLC patients in response to CBD treatment, and that CBD treatment of cisplatin-resistant NSCLC cells is capable of inhibiting tumor growth and metastasis (5).
Figure 1: Hematoxylin and eosin (H&E) staining of murine lung tissue treated with a vehicle control, cisplatin, and cannabidiol (CBD). Upper and lower rows represent micro- and macro-metastases, respectively. © 2022 Misri et al., licensed under CC BY 4.0.
Improving cisplatin-induced organ damage with CBD and CBGA
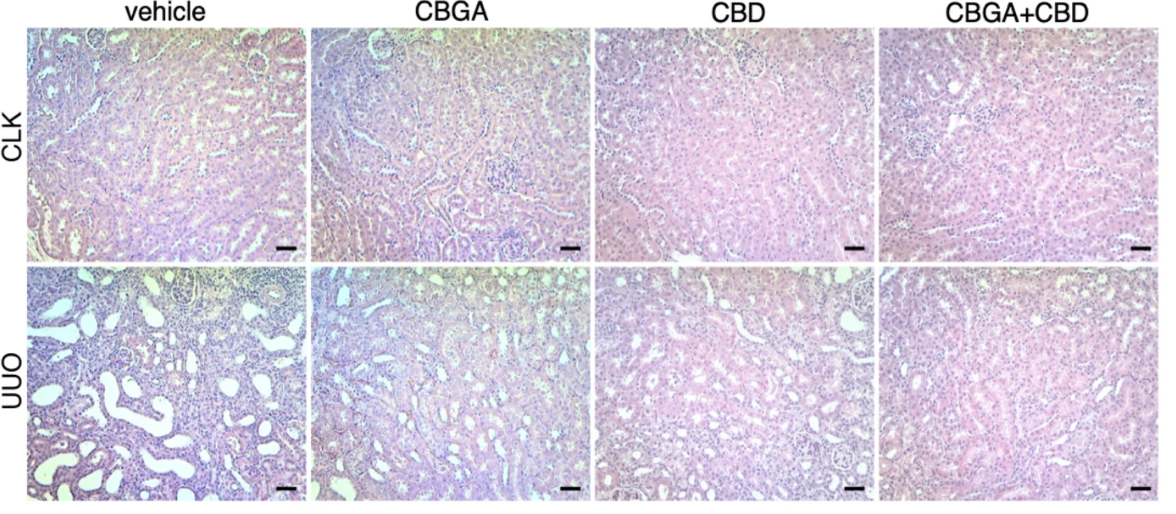
While Misri et al. highlighted the antitumorigenic effects of CBD, a more recent study from Suzuki et al., demonstrated an additional benefit from CBD and other cannabinoid derivatives. Cannabigerol (CBG), the third most prevalent cannabinoid in cannabis, has a similar pharmacological profile to CBD. Additionally, the acidic form of CBG, cannabigerolic acid (CBGA), has been implicated in the regulation of calcium signaling and inflammatory pathways in pro-inflammatory immune cells, indicating its potential to attenuate kidney inflammation. Chemotherapeutics like cisplatin have been shown to cause severe kidney damage, however, as cannabinoid receptors mechanisms have been implicated in kidney disease and damage, CBD/CBGA and their derivatives may have potential therapeutic applications in the treatment of chemotherapy-induced kidney damage. To determine whether CBGA and CBD can attenuate cisplatin-induced kidney damage, Suzuki et al. induced kidney damage using cisplatin and unilateral ureteral obstruction to mimic the physiological setting of acute and chronic nephropathy. Once kidney damage was induced, CBGA, CBD, a combination of both, or vehicle controls were injected into both acute and chronic model mice daily for seven days. Following this injection protocol, mice were euthanized and kidney function and apoptosis were evaluated together with histological and immunohistochemical analysis to fully assess kidney function and damage (6).
CBD & CBGA Attenuates Kidney Damage
Cannabinoids CBGA and CBD were able to reduce kidney damage caused by cisplatin and prevented kidney function deterioration in the chronic setting within a nephropathic mouse model. Both cannabinoids were capable of maintaining kidney function, with no observed reduction in urine output. Both treatments also reduced apoptosis in the cisplatin-induced kidney injury model, and prevented the increase of blood urea nitrogen and creatinine typically observed in mice treated with cisplatin. While both cannabinoids were effective overall, CBGA was most effective at reducing inflammation in the cisplatin-induced setting of nephropathy, demonstrating its potential to protect against kidney damage resulting from inflammation and fibrosis. While not particularly relevant to cisplatin-induced kidney damage, CBD and CBGA were both effective at attenuating kidney atrophy and renal fibrosis in the chronic model, and reducing morphological changes in the unilateral ureteral obstruction model. Ultimately, CBGA appeared to be the most impactful when preventing kidney damage from inflammation and fibrosis in both the acute and chronic setting, whereas CBD prevented the progression of chronic renal fibrosis. As kidney damage is a common side effect of most chemotherapeutics, finding a treatment capable of reducing this that also exhibits antitumorigenic effects is extremely promising (6).
Figure 1: H&E staining of murine kidney tissue experiencing acute (CLK) or chronic (UUO) kidney after treatment with a vehicle control, CBGA, CBD or CBGA and CBD. © 2023 Suzuki et al., licensed under CC BY 4.0.
Limitations of Cannabidiol (CBD) treatment
While these two studies highlight the therapeutic benefits of CBD and CBGA for treating chemotherapy-induced side effects, questions about safety and regulation persist. Research involving CBD was not feasible in the United States until the regulatory requirements were reduced by the FDA in December 2015, thereby limiting available data (4). Additionally, as CBD products are not officially regulated by the government, consumers may not be aware of the specific contents of the therapeutic product they’re purchasing. For example, a recent study from Goulette et al. sought to further understand how informed a subset of cancer patients and survivors (343 participants) were about the cannabis products they were consuming, and found that only 27.2% of the study participants were aware of the Tetrahydrocannabinol (THC) and CBD potency (7). While this does represent a small proportion of the population of cancer patients and survivors that consume cannabis, the data demonstrates that cannabis consumption for medicinal use requires further awareness and regulation to reach its full therapeutic potential.
Conclusions and future directives
The current scientific literature consistently reports that CBD is an effective antitumor agent against certain cancers, including breast cancer and NSLSC (5,8). The vast majority of these publications require further clinical studies to validate their findings; but nevertheless, preliminary clinical research has shown promising. For example, a 2018 study reported a 92% response rate from pharmaceutical-grade synthetic cannabidiol in 119 patients with solid tumors, with beneficial effects including a reduction in tumor size and circulating tumor cells observed in most cases (8). However, most studies that report on the effects of CBD for cancer patients have rather small participant pools, and additional longitudinal, wide-scale studies need to be performed to better understand its effects. Taken together, the benefits of CBD as an anti tumorigenic and a potential therapeutic for the side effects of chemotherapy appear to overshadow any potential negative consequences, but further clinical studies will be required before CBD can be considered a truly effective treatment.
About the Author
About the Author

Jasmin Skinner is an undergraduate student at the University of Western Ontario completing a Specialization in Biology and a Minor in Chemistry, with focused interest in applying these concepts to environmental conservation. As a lover of the outdoors and the arts, much of her time is spent in nature and within the local London art community, creating and connecting with all walks of life. After graduating, she hopes to continue her passion of finding unconventional solutions to environmental issues by working with nature, not against it.
References
- Canadian Cancer Society. Side effects of chemotherapy. Cancer.ca. 2016. Accessed April 2023.
https://cancer.ca/en/treatments/treatment-types/chemotherapy/side-effects-of-chemotherapy - Dasari S, Tchounwou PB. Cisplatin in cancer therapy: molecular mechanisms of action. Eur J Pharamcol. 2015;740:364-378. doi: 10.1016/j.ejphar.2014.07.025
- American Society of Clinical Oncology (ASCO). Topic #2: Chemotherapy with Multiple Drugs Instead of with One Drug for Breast Cancer that Has Spread. Cancer.net. Accessed April 2023. https://www.cancer.net/about-us/collaborations/top-five-list-oncology/choosing-wisely%C2%AE-2013-asco%E2%80%99s-second-list-top-five-tests-procedures-and-treatments-many-patients-do/topic-2-chemotherapy-multiple-drugs-instead-one-drug-breast-cancer-has-spread#:~:text=In%20addition%2C%20patients%20who%20receive,or%20reduce%20the%20side%20effects
- Grinspoon P. Cannabidiol (CBD): What we know and what we don’t. Harvard Health Publishing, Harvard Medical School. September 2021 published. Accessed April 2023. https://www.health.harvard.edu/blog/cannabidiol-cbd-what-we-know-and-what-we-dont-2018082414476
- Misri S, Kaul K, Mishra S, et al. Cannabidiol inhibits tumorigenesis in cisplatin-resistant non-small cell lung cancer via TRPV2. Cancers. 2022;14(5):1181. Doi: 10.3390/cancers14051181
- Suzuki S, Fleig A, Penner R. CBGA ameliorates inflammation and fibrosis in nephropathy. Sci Rep. 2023;13:6341. doi: 10.1038/s41598-023-33507-2
- Goulette M, Schlienz NJ, Case A, et al., Abstract 6472: Self-reported knowledge of Δ9-tetrahydrocannabinol (THC) and cannabidiol (CBD) potency in cannabis products among cancer patients and survivors: Results from a survey of cannabis consumers at an NCI-designated cancer center. Cancer Res 2023;83(7):6472.
https://aacrjournals.org/cancerres/article/83/7_Supplement/6472/720534 - Kenyon J, Liu W, Dalgleish A. Report of objective clinical responses of cancer patients to pharmaceutical-grade synthetic cannabidiol. Anticancer Res. 2018;38(10):5831-5. doi: 10.21873/anticanres.12924
- Seltzer ES, Watters AK, Mackenzie D Jr, Granat LM, Zhang D. Cannabidiol (CBD) as a promising anti-cancer drug. Cancers. 2020;12(11):3203. doi: 10.3390/cancers12113203