In this webinar, Bin Xie, PhD, provides an overview of immuno-oncology drug development, presents different humanized mouse models available for drug evaluation, and discusses imaging mass cytometry for mechanism analysis or biomarker discovery.
Highlights
- Key events in the immuno-oncology (IO) timeline
- Humanized mouse models by LIDE Biotech for IO drug evaluation
- Real-world case studies using these platforms
- Benefits of imaging mass cytometry for IO research
Webinar Summary
To begin this webinar, Dr. Xie first provides a brief overview of key events in the immuno-oncology (IO) timeline, which include the discovery of Coley’s toxin and interleukin-2 for cancer therapy in 1891 and 1983, respectively. However, the clinical potential of these therapies was limited due to consistency and toxicity issues. The first CTLA4 antibody was approved by the Food and Drug Administration (FDA) in 2011 for use in melanoma patients. Shortly thereafter, the PD-1 antibody was FDA-approved for melanoma, lung cancer, and brain cancer treatment.
From 2017 to 2020, there was a 233% growth in the IO drug pipeline, in which efforts were mainly focused on cell therapy, T cell-based immunomodulators, and bispecific antibodies, with top targets including PD-1 and PD-L1. In 2021, an increasing number of novel cancer therapy targets were identified and studied for clinical translation such as ID3/SOX4 and neutrophil elastase. It was discovered that human, but not murine, neutrophils release factors that selectively kill cancer cells. Purified mouse neutrophil elastase can also kill cancer cells, but its function was silenced during its secretion.
“So, it seems helpful for us to directly use humanized mouse models for IO drug tests as it [reflects] the human immune system.”
Dr. Xie next discusses various humanized mouse models that are available for IO drug evaluation. The CD34+/hematopoietic stem cell model is a fully human immune system with delayed or no graft versus host disease (GvHD), but is expensive and time-consuming. The humanized peripheral blood mononuclear cell (huPBMC) model is a popular choice, but due to GvHD, its therapeutic window for IO drug testing is very narrow. Alternatively, huPBMC-cancer cell co-inoculation mimics the tumor-immune microenvironment with delayed or no GvHD, and has been successfully used in many IO drug evaluations.
Many classic and special huPBMC mouse models have been developed and optimized by LIDE Biotech for the evaluation of diverse IO Drugs. For classic donor-selected huPMBC reconstituted mouse models, patient-derived xenograft (PDX) tumor fragments or cancer cells are inoculated in NCG mice, which are reconstituted with huPBMCs and can be applied for antibody efficacy evaluation in vivo. Since PBMC donors have varying T cell reconstitution rates and anti-tumor effects, LIDE Biotech’s unique donor selection method allows for in vivo drug efficacies to be easily evaluated. Dr. Xie also discusses huPBMC-reconstituted PDX models for immunotherapy and provides some case studies in various cancer models.
“As I mentioned before, the therapeutic model of classic PMBC humanized models is narrow … In the last ten years, we have developed human PBMC and cancer co-inoculated mouse models.”
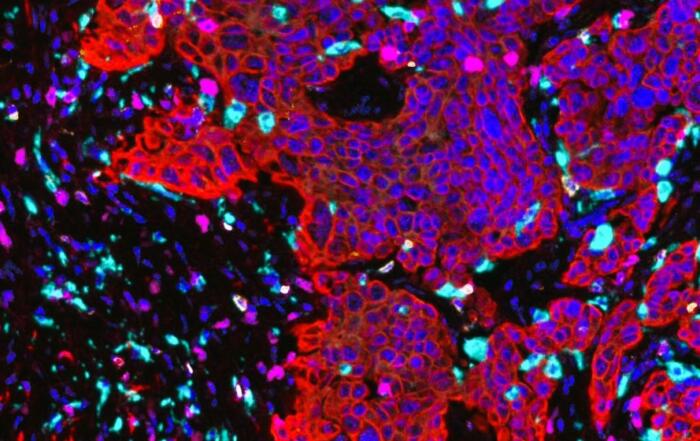
For huPBMC and cancer cell co-inoculation models, huPBMCs and cancer cells are co-cultured in vitro and injected into NCG mice for antibody testing. Immunofluorescent imaging validated that CD3+ T cells were well-infiltrated in tumor tissue while flow cytometry data showed that approximately 3% of CD3+ T cells infiltrated tumor tissue 25 days after co-transplantation. In addition to PD-1 and PD-L1, more diverse targets have been recently identified such as CD155, CD112, TIGIT, and VISTA. As an example, Dr. Xie shows that the huPBMC and A375 melanoma cancer cell co-inoculation model worked well for testing CD73, TIGIT, and GITR antibodies. Additionally, a lung cancer/huPBMC co-transfer model worked well for testing DLL/CD3 bispecific antibodies.
LIDE Biotech’s biobank consists of more than 1600 models that were established in-house. Dr. Xie provides detailed real-world case studies of how these models have been used. For example, PD-L1 expression on cancer cell surfaces was found to be a useful biomarker for PD-1 antibody therapy in vivo; nivolumab demonstrated good efficacy on non-small cell lung cancer (NSCLC) PDX with high PD-L1 expression, but NSCLC PDX with low PD-L1 expression was not sensitive to nivolumab treatment.
Dendritic cells (DCs) are powerful antigen-presenting cells for inducing humanized T cell activation and effective T cell differentiation. Co-inoculation of DCs with autologous T cells and cancer cells demonstrated that the combination of CD40 and PD-L1 antibodies could stop the development of melanoma. M2 macrophages in huPMBC have also been induced in vitro and co-inoculated with autologous PBMCs in tumor-bearing mice for the evaluation of antibody efficacies in vivo; the CD47 antibody has demonstrated a synergistic anti-tumor effect with other antibodies in this model. In parallel with these in vivo studies, LIDE Biotech also offers in vitro platforms for investigating or validating IO drug functions using specific immune cells. Dr. Xie additionally introduced some humanized models with effector immune cells and oncolytic viruses.
“We also have some data … from oncolytic viruses, which could efficiently kill tumor cells by boosting [the] immune system.”
To better understand the mechanisms of IO drugs in vivo, LIDE Biotech has used imaging mass cytometry (IMC) composed of a Hyperion tissue imager for capture and Helio cytometry by time-of-flight (CyTOF) for detection and quantification. In IMC a tissue section stained with multiple heavy metal-labeled antibodies is loaded into the Hyperion and quantified by the Helios system. IMC can also run PhenoGraph clusters for tumor tissue heterogeneity assessment to help clinicians identify which cell subsets are sensitive or resistant to PD-1 antibody therapy. Now, up to 29 and 47 markers are ready-to-go for CyTOF and IMC panels, respectively.
“IMC is such a powerful tool that it allows us to gain an appreciation of the heterogeneity in tissue … function and assess complex phenotypes and tumor-immune [cell] interactions in [the] tumor microenvironment.”
Lastly, Dr. Xie summarizes the IO platforms that are available on the market. LIDE Biotech has built stable and well-tested humanized mouse models for IO drug testing in vivo and in vitro, as well as analytical platforms including conventional flow cytometry and tissue IMC. Dr. Xie concludes the webinar by highlighting that LIDE Biotech provides a one-stop solution for IO research, drug development, and cancer drug evaluation.
Click to watch the webinar recording. To view the presentation full screen simply click the square icon located in the bottom-right corner of the video viewer.
Resources
Q&A
- Is it possible to use customized antibodies instead of the standard panel antibodies?
- How do you determine the ratio of immune versus cancer cells in your co-injection models?
- Are you planning on expanding targets or will it just be customized studies beyond those 12 that are already available?
- Is your humanized PMBC mouse model stable and how is the reproducibility of the assay system?
- Do you have labs in the United States that can perform these studies?
- What are the humanization percentages that you usually get with your models?
To retrieve a PDF copy of the presentation, click on the link below the slide player. From this page, click on the “Download” link to retrieve the file.
Presenters
Director of Immuno-oncology
LIDE