Dr. Andrea Bonetto discusses the importance of musculoskeletal preservation in cancer treatment and shares evidence that bone protection directly impacts muscle size and function in cachexia.
Highlights
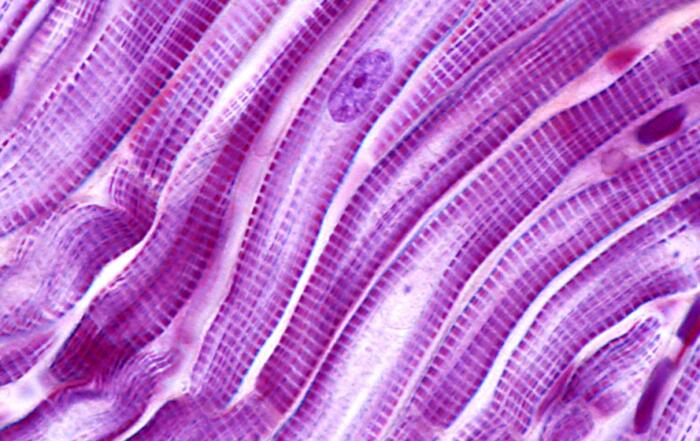
- Overview of cachexia and importance of preserving skeletal muscle
- A comparison of cachexia resulting from cancer versus chemotherapy
- Bone and muscle crosstalk in cancer and chemotherapy
- The role of RANKL (Receptor activator of nuclear factor kappa-Β ligand) in cachexia
Webinar Summary
Dr. Bonetto begins the webinar with an introduction to cachexia, a comorbidity of several chronic diseases including cancer. Cachexia causes reduced response to cancer treatments, severe weight loss exacerbating mortality rates, and accounts for roughly one third of cancer deaths. He explains that preservation of skeletal muscle mass has been shown to prolong survival in tumor hosts, and patients with higher muscle mass are more resistant to chemotherapy with better overall outcomes. Unfortunately, while chemotherapy is currently the preferred treatment, it continues to result in muscle weakness and fatigue in survivors.
The Bonetto group has investigated whether chemotherapy and cancer are able to drive musculoskeletal atrophy and muscle weakness through similar mechanisms. They found that cancer affects muscle function in both male and female mice, and the animals had reduced overall activity; additionally, chemotherapy treatment also caused skeletal muscle wasting and weakness. However, they discovered cachexia in C26 mice (an animal model of colon carcinoma) and chemotherapy-induced cachexia activated different pathways. Further, cancer and chemotherapy also both caused mitochondrial dysfunction in muscle.
“. . . when we compared these effects in animals exposed to chemotherapeutics, we observed activation on different signalling pathways, suggesting that despite similar phenotypes, the mechanisms were likely different.”
While muscle loss is a hallmark of cachexia, there is evidence that bone is also affected. Dr. Bonetto explains that cancer cachexia is a multi-organ disorder; imbalances in bone and muscle-derived biochemical factors may play a role in its pathogenesis. He continues with an overview of various studies investigating whether bone-targeting therapies preserve skeletal muscle in cachexia.
“Muscle and bone cross-talk has historically been very well investigated in terms of mechanical interaction. . . however, biochemical communication has been neglected for a longer time. . . “
Bone homeostasis is normally regulated by a balance between bone formation and bone resorption. Another important question is whether RANKL, the soluble factor that binds to the surface of osteoclast precursors, was being secreted directly by the tumors. RANKL has been found to play a role in regulating muscle mass, and the next series of studies presented revealed that it promotes muscle atrophy and that high RANKL is sufficient to cause muscle and bone loss.
Dr. Bonetto concludes the webinar by highlighting the following key points: growth of non-metastatic cancers can result in bone loss, RANKL is a regulator of muscle size in cachexia, and anti-resorptive strategies protect from muscle and bone loss in cancer or after chemotherapy.
Resources
Q&A
- Is altered mitochondrial morphology due to cancer and chemotherapy also the result of changes to mitochondrial homeostasis? If so, are there any available tools to prevent the loss of mitochondria in skeletal muscle and would these prevent the loss of muscle mass and strength?
- How early do the cachexia events start during cancer development?
- Bone, muscle, and adipocytes come from the same stem cell origin – do adipocytes have to be added to this scenario?
- What types of assays do you use to characterize cachexia and do you ever look at the metabolic function of the muscle in vitro, glucose uptake, etc.?
- Is there evidence for RANKL upregulation following chemotherapy?
- In bone cells, RANKL signals via the PI3K-Akt pathway, a well known anabolic signalling pathway in skeletal muscle, yet RANKL appears to cause muscle atrophy. Can you speculate what the basis is for this contradiction?
- Does RANKL have direct effects on muscle receptors?
- What is the relevance of in silico studies for understanding cancer-associated cachexia?
- Your data suggests that ovarian cancers are the primary source of RANKL – does bone-derived RANKL also play a role in driving skeletal muscle wasting in your animal model?
- Can you explain why in some of the force frequency curves, you see higher frequencies causing lower torque production than the moderate frequencies?
- Does the CRC metastasize to bone and are they osteogenic or osteolytic?
- Exercise has been proposed as a therapy for muscle wasting due to cancer cachexia – are adverse effects less in physically active patients before starting therapy?
- How does the quantity of bone loss in the RANKL-expressing C26 model compare with the other established cachexia models? Is the lack of a skeletal phenotype in a normal C26 model due exclusively to low RANKL-expression or are there other reasons why this model exhibits no bone phenotype?
- Does RANKL have a role in cardiac function in your model of cachexia?
To retrieve a PDF copy of the presentation, click on the link below the slide player. From this page, click on the “Download” link to retrieve the file.
Presenters
Associate Professor
Surgery
Indiana University