In this webinar, Dr. Emma Karey presents evidence of the first- and second-hand exposure risks of vaping, discusses how public perceptions influence e-cigarette usage, and provides a translational framework for integrating scientific principles and novel conditions.
Highlights
- Timeline of cigarette and e-cigarette regulations in the United States
- Evidence of unique respiratory risks of vaping
- Second-hand effects of cigarette vs. e-cigarette emissions
- How public perceptions influence smoking vs. vaping
- How to adapt the science to address this quickly evolving field
Webinar Summary
Dr. Karey begins this webinar with a brief history of smoking, the rate of which has been steadily declining since 1954. Although the first evidence linking smoking with lung cancer emerged in 1957, the Surgeon General report was not published until 1964. While scientists and medical professionals have since agreed that cigarettes are harmful, smoking prevention and tobacco control policies have only emerged in the past decade. In 2016, the Food and Drug Administration (FDA) was able to expand the definition of tobacco products so that they could also govern e-cigarettes for the first time. The FDA banned flavored e-cigarette rechargeable cartridges in 2020, but a loophole in the law allows for their sale as long as they are disposable or the nicotine is synthetic.
“In all fairness, it’s not just the federal regulators that are playing catch-up. The scientific community, myself included, struggles with this as well.”
E-cigarettes are evolving so quickly that by the time data are published, the findings are old or outdated. While vaping may have started as a form of harm reduction for cigarette smokers, e-cigarette usage has surpassed traditional cigarette usage in teenagers. Consequently, research focus has shifted towards why e-cigarettes are so appealing to adolescents and whether vaping puts these individuals at an elevated risk of adverse respiratory effects.
Toxic chemicals have long been detected in e-liquids and vaping emissions. Flavors have been the main focus of e-cigarette toxicity research and regulatory efforts since it is believed that they contribute to the appeal of e-cigarettes. However, several other sources of toxicity have been identified, including the nicotine itself, heavy metals from coils, pyrolysis of sugar-based solvents, and battery output voltage. Many public health outlets and tobacco industries have framed vaping devices as safer alternatives to traditional cigarettes, but these two nicotine delivery methods differ more than they overlap.
“Several factors make it difficult to conduct an apples-to-apples comparison in my opinion, either between [e-cigarette] studies alone, or when assessing relative vaping and smoking risks, including a lack of standardized parameters in all of our studies, assessment and identification of relevant endpoints, and … [population] selection.”
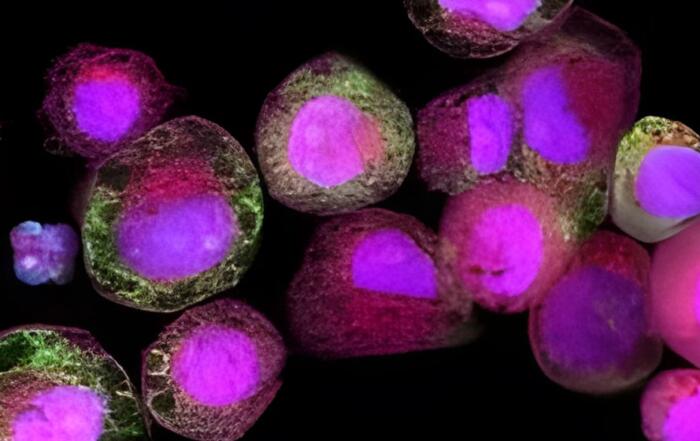
In the next portion of this webinar, Dr. Karey discusses the unique respiratory risks of vaping. In one study, Dr. Karey and colleagues quantified nasal and oral cavity inflammation in vapers, smokers, and tobacco-free individuals. Interestingly, 9 out of 10 cytokines that were assayed were elevated in the noses of vapers compared to the control group, but none of these cytokines were elevated in the noses of smokers. Salivary cytokines were comparable in smokers and vapers, suggesting that vapers and smokers are using these products to achieve similar blood nicotine levels.
“How you use a product, even when the constituents are the same, … can affect your health risks.”
Vapers tend to exhale from their nose in addition to their mouth, which is known as retrohaling. In another study, Dr. Karey observed that vapers are three times more likely to retrohale than smokers and four times more likely to exclusively exhale from their nose. Retrohaling may appeal more to vapers than smokers since it has been reported to greatly enhance flavor.
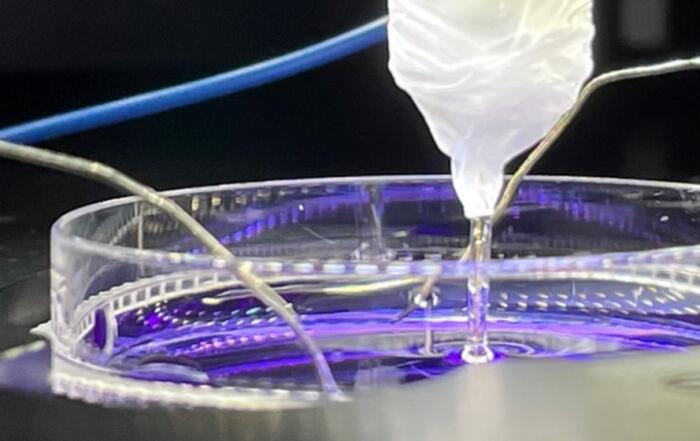
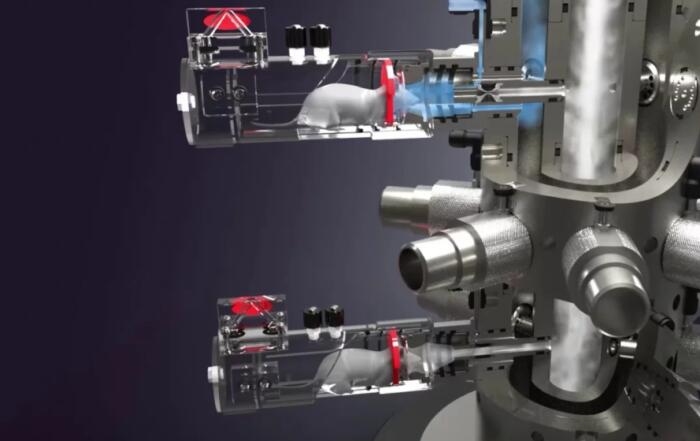
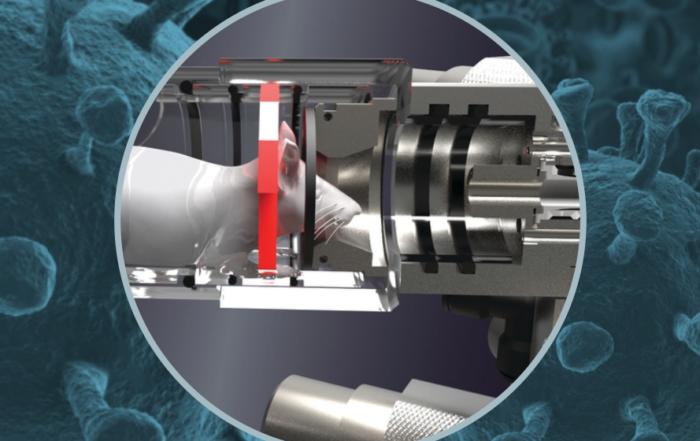
Dr. Karey next discusses the second-hand effects of tobacco emissions; an estimated 2.5 million non-smoker deaths are attributed to second-hand smoke (SHS) exposure, and approximately 75% of SHS-related morbidities are cardiovascular. Although many pathways are known to be affected by SHS, Dr. Karey focuses on autonomic dysfunction. To study the long-term consequences of SHS, Dr. Karey monitored heart rate variability (HRV) in rodents over 12 weeks using HD-X11 telemetry devices by Data Sciences International. Since HRV decreases are associated with an increased risk of arrhythmias, Dr. Karey also performed stress tests on the rodents and monitored pre-ventricular contractions (PVCs).
Following four weeks of SHS exposure, modest decreases were observed in overall and intermediate HRV, while a dramatic decrease was seen in short-term HRV. Stress-mediated increases in arrhythmias were also observed in both SHS and control groups, but these levels recovered post-restraint. After 12 weeks, dramatic decreases were observed in all HRVs in SHS-exposed mice, but a similar trend was observed in PVCs compared to the 4-week point. Dr. Karey’s colleagues explored other SHS-related mechanisms using the same mouse cohort, and discovered a reduced excitability of cardiac vagal neurons which could explain the observed HRV reduction, while others found evidence of endothelial dysfunction.
“This is why smoking bans are important and why we need legislation restricting environmental tobacco smoke.”
In the final portion of this webinar, Dr. Karey discusses how public perceptions may impact actual risks. A study that polled dual users of e-cigarettes and traditional cigarettes found that vaping is preferred over smoking around loved ones, suggesting that e-cigarettes are perceived to be safer than traditional cigarettes. In a study of indoor air quality, colleagues of Dr. Karey’s measured pollutant concentrations in tobacco-free homes as well as the homes of vapers and smokers. On average, 22 times more particulate matter (PM) was found in the homes of smokers compared to tobacco-free homes after approximately 22 minutes of smoking, while 66 times more PM was found in the homes of vapers compared to tobacco-free homes after 47 minutes of vaping. Dr. Karey further notes that the perceived safety of e-cigarette consumption could explain this longer average indoor vape time.
“How do we adapt our science to address this … evolving field?”
Dr. Karey explains that there are four toxicology aphorisms to address this question. The first is a precautionary principle: since science does not always adapt quickly enough to establish absolute cause and effect, one should use common sense. Furthermore, researchers should consider endpoint selection, as the degree of exposure has a direct relationship with the magnitude of harm. Studies should also be adjusted to mirror the changing conditions of this field and reflect real-world exposure. Lastly, Dr. Karey recommends thinking outside the box, as using established techniques and approaches to study something new may not always result in the answers that are needed.
“When in doubt, look to the product users, or at least check out what they’re saying on Reddit. … They’re pretty candid and honest and give you a lot of information. … We should be referencing them and taking what they say with more than just a grain of salt.”
Importantly, tobacco messaging must be contextualized and improved: if vaping is said to be less harmful than cigarettes, it may be interpreted as not harmful at all. Multiple comparators aside from cigarettes should be considered to include people who do not consume tobacco. Lastly, a new generation of vaping devices known as “heat-not-burn” devices are beginning to roll out; these devices essentially equate to vaping a cigarette, the consequences of which are not yet known. Dr. Karey concludes that researchers must be creative in adapting the science to keep up with this ever-evolving field.
Click to watch the webinar recording. To view the presentation full screen simply click the square icon located in the bottom-right corner of the video viewer.
Resources
Q&A
- Can you go into more detail on what information SDNN provides that the others do not?
- Have you assessed neighbor smoking habits?
- Did you use a nasal swab to get the cytokine concentration?
- Has anyone found an association between sinus or nasal polyposis and vaping?
- Are you aware of any correlation between vaping and allergy?
To retrieve a PDF copy of the presentation, click on the link below the slide player. From this page, click on the “Download” link to retrieve the file.
Presenters
Postdoctoral Research Fellow
Environmental Medicine
NYU Grossman School of Medicine