Dr. Merry Lindsey discusses her research examining the physiology of recovery from cardiac events. Age plays a pivotal role in the deterioration of cardiovascular functionality, resulting in an increased risk of cardiovascular disease in older adults, including atherosclerosis, stroke, and myocardial infarction.
Highlights
- An introduction to myocardial infarction (MI)
- Macrophage, neutrophil, and fibroblast signaling after MI
- Exogenous interleukin-4 (IL-4) treatment in a model of MI
- The role of matrix metalloproteinases (MMPs) in MI
Webinar Summary
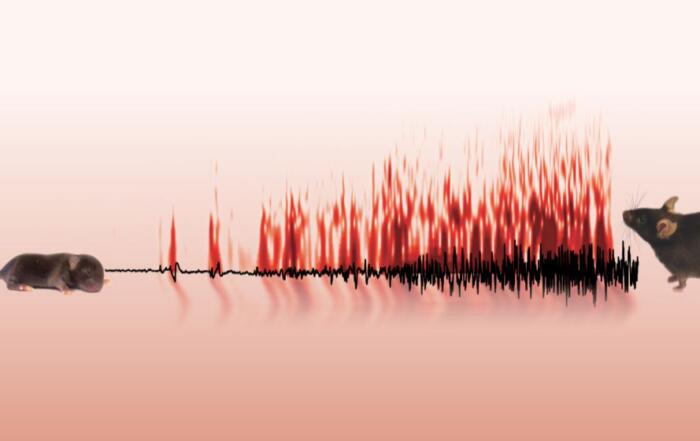
Dr. Lindsey begins this webinar with an introduction to MI, including electrocardiogram (ECG or EKG) traces, histological changes, and the MI response time course; her lab is particularly interested in studying the balance between destruction of the existing extracellular matrix (ECM) and the construction of new ECM resulting in scar formation. Macrophages, neutrophils, and fibroblasts play an important role after MI, and the signaling networks of these different cell types are described in relation to pathophysiology during the first week after infarction.
Low levels of IL-4 are expressed following MI, but IL-4 receptor (IL-4r) expression increases in both macrophages and fibroblasts. This led to the hypothesis that exogenous IL-4 applied 24 hours after MI would promote a polarization switch in inflammatory cell phenotypes. The experimental protocol for investigating this hypothesis is described, including baseline ECG assessment, MI surgery and IL-4 pump implantation, followed by terminal assessment.
“. . . combined, these factors work together to increase inflammation resolution and accelerate the transition to the reparative phase when IL-4 is presented exogenously.”
Exogenous IL-4 resulted in significantly reduced tissue expression of the pro-inflammatory markers CCL3, IL-12a, TGFβ1, and TNFα at day 3 following MI, although some pro-inflammatory and anti-inflammatory markers did not decrease, likely as a result of IL-4 application beginning 24 hours after MI. The anti-inflammatory macrophage markers Arg1 and Ym1 were increased by day 3 after MI, however none of the pro-inflammatory markers were increased, suggesting that IL-4 promoted conversion of M2 macrophages. Immunohistochemistry of isolated macrophages revealed that IL-4 stimulated increased uptake of neutrophil components, consistent with phagocytosis of neutrophils, and study of ex vivo and in vitro phagocytic gene expression by macrophages identified genes involved in this process. A summary of the effects of IL-4 on macrophages in vivo is presented, collectively illustrating a shift towards inflammation resolution and transition to a reparative phase.
“Every MMP has some common features with other MMPs but also some distinct novel characteristics that set it aside from the other MMPs.”
In the next portion of this webinar, Dr. Lindsey describes cardiac metalloproteinase action (CarMA) postulates as developed by her lab and supported with evidence. Dr. Lindsey’s lab has contributed the MMP-9 CarMA knowledge map, illustrating the inflammatory mediators produced following MI and other signaling pathways involved in phagocytosis, apoptosis, and scar formation. The role of MMP-12 after MI is also introduced, including evidence that MMP-12 inhibition worsens left ventricular geometry and physiology, associated with late ECM degradation and prolonged inflammation; these results suggest a possible protective role for MMP-12 after MI.
“Even though something goes up doesn’t mean that inhibition is the optimal strategy for therapeutic options . . . sometimes factors are going up after MI as a way to serve a cardioprotectant role . . . to be a resolution promoting factor.”
To conclude the webinar, Dr. Lindsey discusses the role of MMPs in MI, and the importance of understanding the relationship between inflammation and fibrosis in remodeling to help identify at-risk patients that may benefit from early and aggressive therapy.
Resources
Q&A
- Is infarct confirmed at the time of ligation by visual inspection and blanching?
- Have you observed differences based on sex of the mice?
- Does IL-4 alter checkpoint signaling?
- Does IL-4 affect cardiac myocytes?
- Are the N2 neutrophils observed at day 5 to 7 a newly recruited population?
- How does the MI environment change with aging?
- Do you measure enzyme MMP activity, and if so, what is your preferred method?
- How are T cells involved in the remodeling process?
- Is there evidence that exercise is protective against MI?
- Is it possible to use stem cells for repair after MI?
- Is IL-13 likely to have similar effects to IL-4?
- Would you expect differences when using a permanent occlusion model as opposed to a ischemia-reperfusion model?
- Did IL-4 treatment result in functional improvement?
- How would metabolic syndrome or preexisting systemic inflammation affect the macrophage response?
- How do changes in cardiac inflammation post-MI contribute to differences in cardiac metabolism and vice versa?
- Can reperfusion after ischemia alter the time course of the inflammatory and reparative processes?
- Where do you see this field heading in the next 10 years?
To retrieve a PDF copy of the presentation, click on the link below the slide player. From this page, click on the “Download” link to retrieve the file.
Presenters
Chair
Cellular and Integrative Physiology
University of Nebraska Medical Center