In this webinar, Professors Julio Ayala and Matthew Robinson discuss the effects of comfort feeding, stress, and exercise on metabolism and obesity in mouse models.
Highlights
- Relationship between stress and obesity
- Mechanisms that underlie stress-induced hypophagia in mice
- How obesity impacts skeletal muscle physiology, particularly mitochondria
- Effect of exercise on substrate oxidation
Webinar Summary
Professor Ayala begins this webinar by addressing the relationship between stress and obesity. Since 2005, there has been a substantial increase in the prevalence of American adults with a high body mass index (BMI), a marker for obesity. Feelings of stress are also on the rise, particularly in the last year due to the COVID-19 pandemic as well as social and political unrest. Professor Ayala emphasizes that this parallel rise does not prove that there is a direct relationship between obesity and stress. However, it is well-documented that stress can affect behaviors that lead to weight gain, such as caloric intake and food restriction. A majority of individuals, regardless of gender, report that they increase their caloric intake in response to stress through snacking. Unsurprisingly, these snacks tend to be unhealthy, and usually comprise foods that are high in fat and sugar.
“This has given rise to the terms “comfort food” and “comfort feeding” which refer to the increased consumption of palatable, highly caloric substances based on the rewarding and soothing properties mitigating the negative feelings associated with stress.”
Interestingly, comfort feeding can be mimicked in preclinical rodent models. The typical response of rodents to a stressor is decreased food intake (i.e., hypophagia); however, studies have shown that when presented with a palatable substance such as sucrose or a high fat dye, hypophagia is either attenuated or lost completely. The majority of these studies have been conducted in lean rodents, and while this has led to important discoveries of how stress may promote obesity, much less is known about stress-related behaviors and mechanisms that are relevant when obesity has already been established. A recent study that assessed emotional eating in response to social isolation during the COVID-19 pandemic found that individuals with a high BMI were more likely to engage in maladaptive coping than individuals with a low or moderate BMI.
“Obese individuals are more susceptible to stress and more prone to increase their caloric intake in response to stress.”
Professor Ayala’s goal is to determine how stress influences energy balance parameters that can affect body weight in lean and obese mice, and to explore how obesity itself affects the mechanisms that regulate feeding in response to stress. In the first study presented, mice were placed on a 60% high fat diet (HFD) for several weeks to induce obesity while lean mice were fed a regular diet. To induce stress, mice were placed in a restrainer for one hour, and a Promethion system was used to measure energy expenditure, food and water intake, substrate oxidation, and activity. Restraint stress only reduced food intake in lean mice, while energy expenditure and fat oxidation were stimulated in both lean and obese mice. Locomotor activity was also reduced in both lean and obese mice in response to stress, while water intake remained unchanged
The Ayala research group is also interested in the metabolic actions of the hormone glucagon-like peptide-1 (Glp1), which is secreted by the gut in response to food intake. Glp1 engages a Glp1 receptor (Glp1r) in pancreatic beta cells to stimulate insulin secretion. There are neurons in the hindbrain that produce Glp1, and Glp1r is widely expressed throughout the central nervous system in multiple areas that regulate feeding behavior. Many researchers have shown that stress-induced hypophagia requires brain Glp1 action, and blocking Glp1r in the paraventricular hypothalamus (PVN), bed nucleus of the stria terminalis (BNST), and lateral septum (LS) suppresses the caloric intake reduction observed in lean mice in response to stress.
With a focus on the LS, the Ayala research group investigated whether this system is impaired in obese mice, and if it can explain why obese mice are resistant to stress-induced hypophagia. Data revealed that obesity is characterized by reduced activation of Glp1r neurons in the LS as well as attenuated stress-induced hypophagia. The group also focused on the cannabinoid receptor agonist 2-arachidonoyl glycerol (2-AG) as a cause and/or consequence of impaired Glp1 action in the LS. 2-AG levels in the LS were significantly elevated in obese mice only, which could explain why neuronal activity is dampened in response to stress in these mice and why they are resistant to stress-induced hypophagia. Interestingly, chronic stress stimulates energy expenditure and fat oxidation in both lean and obese mice, suggesting that these phenotypes are regulated by mechanisms other than Glp1r neurons in the LS. Professor Ayala is currently studying these mechanisms further, and is also interested in whether these mechanisms are relevant in other brain regions such as the PVN and BNST.
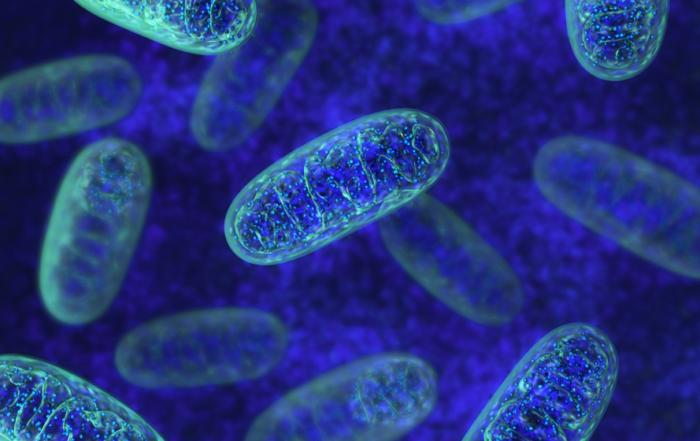
In the second half of this webinar, Professor Robinson discusses the impact of obesity on skeletal muscle physiology with a focus on mitochondria. Obesity is a major risk factor for the development of insulin resistance and type 2 diabetes, the latter of which currently affects approximately 10% of Americans. As obesity prevalence increases, approximately 30% of Americans are projected to develop type 2 diabetes by 2050, creating major personal and public health burdens.
“At those rates, within this one-hour webinar, about 190 people will be newly diagnosed [with type 2 diabetes].”
Sedentary lifestyles and obesity pose many challenges for skeletal muscle. Low exercise means less calories are burned, increased nutrient intake results in fat mass accumulation, and circulating insulin levels subsequently increase to compensate for high blood sugars. Professor Robinson explains that mitochondria are at the center of this process using a roadway analogy: the mitochondria are the main site for substrate oxidation and energy production, so low energy demands and high nutrient pushes result in a “metabolic traffic jam.” While a person can have low mitochondria (i.e., a flaw in the roadway) and be more susceptible to diabetes development, this overt dysfunction is not required for diabetes development.
Professor Robinson explains that there are multiple “on ramps” onto the metabolic roadway from different substrates, which can be broadly classified as either lipid or non-lipid. Non-lipid substrates provide reducing equivalents that enter the electron transfer system (ETS) through complex I, complex II, and glycerol phosphate dehydrogenase, while lipid substrates generate reducing equivalents which enter the ETS through the electron transfer flavoprotein (ETF) with complex I. Since lipid oxidation is related to diabetes development, Professor Robinson focuses on how exercise and obesity regulate oxidation through the ETF, and how exercise can stimulate protein breakdown and synthesis (i.e., protein turnover) to mitigate mitochondrial dysfunction.
“We will be discussing aspects of how [protein turnover] can help shift our broken or rusty mitochondria into these well-oiled machines.”
The Robinson group focused on mitochondrial respiration by isolating mitochondria and performing high resolution respirometry, allowing them to use specific substrates to test various “on ramps” onto the metabolic roadway. Mice were fed a 60% HFD for four weeks to induce obesity, and exercise training was performed for an additional eight weeks. Independent of exercise, obese mice exhibited greater lipid oxidation in both absolute units and relative to protein content compared to lean mice. Therefore, improvements in oxidative phosphorylation capacity in the obese mice could be due to an intrinsic remodeling of mitochondria rather than increased total protein abundance. Professor Robinson next sought to determine how protein turnover contributes to the observed changes in the mitochondrial proteome and whether mitochondrial adaptations with exercise depend on autophagy activation.
Exercise stimulates protein breakdown through autophagy, partly through the Beclin-1/B-cell lymphoma 2 (Bcl2) complex. The Robinson group assessed this pathway using the same HFD/exercise paradigm introduced previously, but with Bcl2 transgenic mice; however, Bcl2 did not seem to be required for any mitochondrial adaptations. Rather than focusing on protein degradation, the Robinson group next investigated the contribution of synthesis to protein turnover. They hypothesized that Bcl2 was operating via a compensatory pathway that could account for adaptive mitochondrial responses, and so their focus shifted to alternative autophagy activation through Parkin. Results from this study showed that Bcl2 transgenic mice indeed exhibited an increase in Parkin localization to their mitochondria. Having established that exercise is a strong way to stimulate mitochondrial remodeling, the Robinson group next aimed to translate these findings to humans.
To determine how mitochondria adapt to fuel oxidation demands during aerobic exercise, volunteers underwent two weeks of high-intensity interval training (HIIT). Meal tolerance tests and isolated mitochondrial respiration measurements were performed to assess whole-body substrate oxidation. A shift in whole-body fuel reliance was observed after a meal in both pre- and post-training; however, in the resting state post-training, participants were oxidizing more lipids than during pre-training. No change in the sensitivity of mitochondria to lipids was observed post-training, but there was a trend towards greater lipid oxidation capacity. Based on evidence suggesting that mitochondria can be overloaded when many competing substrates are present, Professor Robinson next plans to investigate how substrate competition occurs among different nutrients.
Click to watch the webinar recording. To view the presentation full screen simply click the square icon located in the bottom-right corner of the video viewer.
Resources
Q&A
- Did the locomotor activity measures include wheel running behaviors?
- Is it possible that mitochondrial capacity differs among tissue groups?
- How does restraint stress compare to other forms of stress?
- Is the natural exercise regime in mice analogous to HIIT in humans?
- Do obese mice have lower neural response to restraint because they’re “fat and happy?”
- Have you measured reactive oxygen species production in the oxygraph with either substrate?
To retrieve a PDF copy of the presentation, click on the link below the slide player. From this page, click on the “Download” link to retrieve the file.
Presenters
Associate Professor
Molecular Physiology & Biophysics
Vanderbilt University
Assistant Professor
Kinesiology
Oregon State University