Protocol Preview: Creating an Artificial Human Thymus in Mice
Blog post by Jasmin Skinner
Have you ever wanted to model T cell immunity in mice? In this blog post, we review a recent publication from Nature Methods outlining the methodology behind creating an artificial human thymus in humanized mice [2].
Problems with modeling the immune response in mice
Immunodeficiencies, whether present from birth or acquired throughout life, can be debilitating diseases that severely reduce quality of life. These faulty immune responses can result from a dysregulation of the thymus, a gland primarily responsible for the maturation of lymphocytes. While effective treatments exist for a few immunodeficiency disorders, the majority of treatment options are temporary fixes, in part due to a lack of preclinical models that can accurately predict immune responses in humans [1]. However, a novel model recently published in Nature Methods has potential to greatly improve future immune response studies [2].
Join Amanda Vanden Hoek, PhD, and Vesna Posarac, MSc, as they present two novel platforms for the efficient isolation of immune cells from large volume samples. WATCH NOW
Modeling T cell immunity in humanized mice
Mice have long been proven to be invaluable for modeling various aspects of human health, in part due to our physiological similarities. Hematopoietic humanized mice take these similarities a step further. These humanized mice are generated by engrafting human hematopoietic stem cells into immunocompromised mice. It’s not a perfect process though, and modeling T cell immunity in humanized mice has many limitations. Human T cells that mature in a mouse thymus are not able to interact with other human immune cells, which vastly impairs immune function.
Some current solutions for modeling T cell immunity in mice require transplantation of human fetal thymus, which poses ethical concerns and may not be practical for research. Zeleniak et al. have instead proposed a novel method for engineering an artificial human thymus, developed from human induced pluripotent stem cells (iPSCs), for transplantation into hematopoietic humanized mice.
Creating an artificial human thymus
Two major cell types are present in the thymus: transient developing T cells, which originate from hematopoietic progenitor cells (HPCs), and thymic epithelial cells (TECs). TECs are critical for thymus function, as they regulate T cell differentiation and maturation, but are very difficult to acquire. To circumvent this issue while ensuring appropriate thymus function, Zeleniak et al. induced differentiation of thymic epithelial progenitor cells (TEPCs) from human iPSCs. To form the 3D thymus shape, Zeleniak et al. decellularized a mouse thymus, leaving behind only the extracellular matrix. This thymic scaffold was then repopulated with TEPCs and HPCs, and 3D alginate encapsulation technology was used to ensure adequate TEPC differentiation (Figure 1).
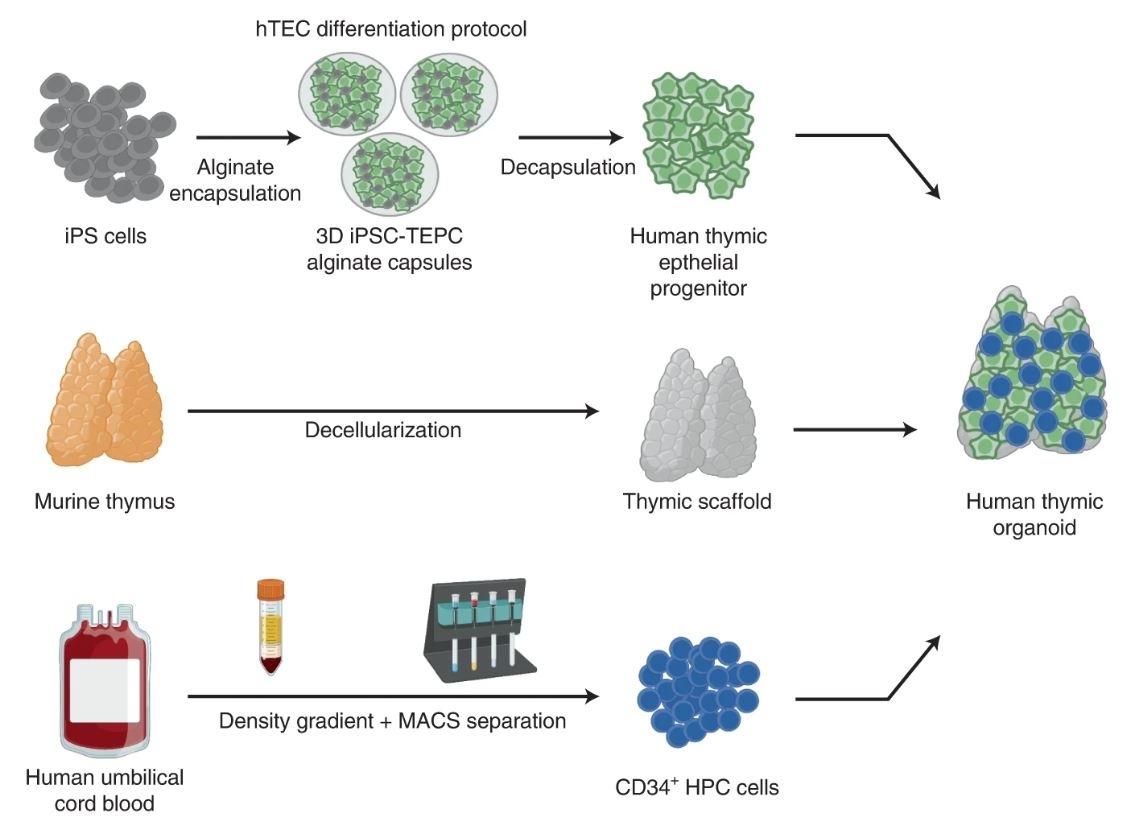
Figure 1: Workflow of artificial human thymus generation. TEPCs are induced from iPSCs in a 3D hydrogel platform, mixed with CD34+ HPCs, which is then injected into a decellularized mouse thymus. © 2022 Zeleniak et al., licensed under CC BY 4.0.
Was the artificial human thymus functional?
The artificial human thymus supported the maturation of the T cell lineage in vitro, with key markers of T cell development being substantially higher in 3D iPSC-TEPCs than those formed from 2D differentiation (Figure 2). Analysis of the humanized mice with the artificial human thymus showed development of a diverse population of human T cells capable of expressing the repertoire of T cell receptors. This was further supported by the restoration of T cell-mediated immune responses, indicating a functional human T cell compartment was successfully created.
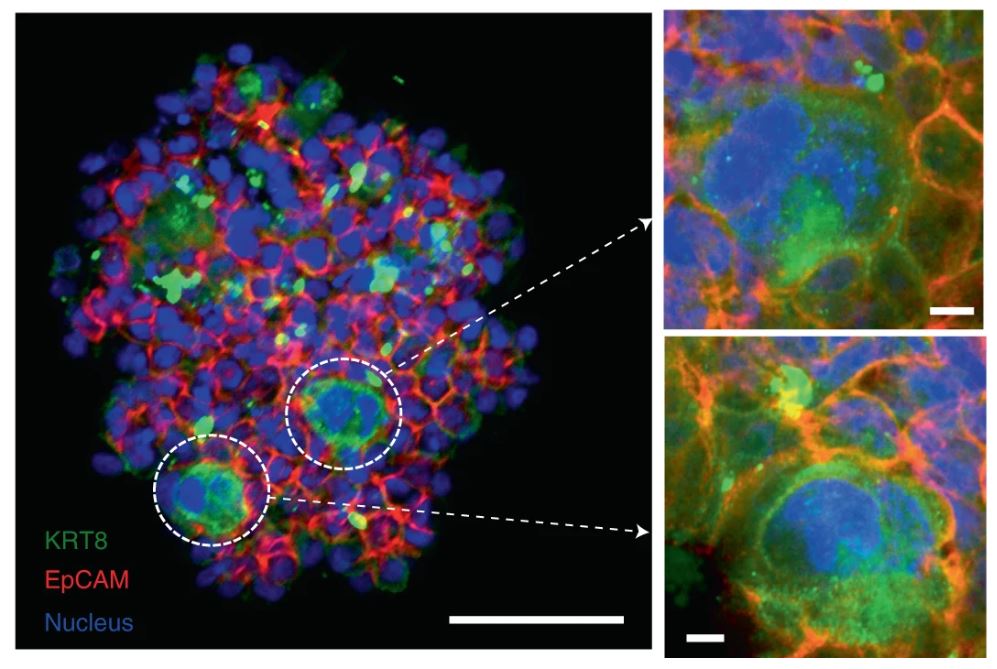
Figure 2: Immunofluorescent images of iPSC-TEC marker aggregates in an artificial human thymus. Scale bars = 50 μm (left), 5 μm (right). © 2022 Zeleniak et al., licensed under CC BY 4.0.
Benefits of a novel immunological model for T cell maturation
While this methodology is far from perfect, it does present many interesting opportunities to study adaptive immune responses. Little is currently known about what causes autoimmune and immune deficiency disorders, and this novel model presents a viable and safe method to study such disorders in vivo. As these organoids are developed from human iPSCs, they also present an opportunity to analyze a wide variety of patient phenotypes. These artificial thymuses could potentially lead to personalized medication based on a patient’s biochemical composition, allowing for a greater range of treatment options.
Could an artificial thymus replace a faulty human thymus?
At present, this organoid model would need further refinement to be considered fully functional. Zeleniak et al. write that the artificial thymus would require further cellular reorganization to improve its function, namely repopulating specific TEC subsets in the appropriate region of the thymus. The authors also seek to improve interactions between T cells and B cells to more accurately model the human immune response within the mouse model.
About the Author
About the Author

Jasmin Skinner is an undergraduate student at the University of Western Ontario completing a Specialization in Biology and a Minor in Chemistry, with focused interest in applying these concepts to environmental conservation. As a lover of the outdoors and the arts, much of her time is spent in nature and within the local London art community, creating and connecting with all walks of life. After graduating, she hopes to continue her passion of finding unconventional solutions to environmental issues by working with nature, not against it.
References
- Brodin P. New approaches to the study of immune responses in humans. Hum Genet. 2020;139:795–9. DOI: 10.1007/s00439-020-02129-3.
- Zeleniak A, Wiegand C, Liu W, McCormick C, Ravikumar K, Alavi A. De novo construction of T cell compartment in humanized mice engrafted with iPSC-derived thymus organoids. Nat Methods. 2022;19:1306-19. DOI: 10.1038/s41592-022-01583-3.
