Q&A Report: Functional Recovery of the Musculoskeletal System Following Injury – Leveraging the Large Animal Model
Answers provided by:
Sarah Greising, PhD
Associate Professor
Kinesiology
University of Minnesota
How important is the location of the injury to the outcome? In particular, in terms of damage to the vascular system as well as nerve branches.
There is not strong data on location of the injury, but it will of course impact the severity of functional loss. I suspect that injuries located at the immediate insertion of the terminal nerve would be more severe than others. Similarly, injuries near the myotendinous junction could also be more impactful, even if the volume lost is similar.
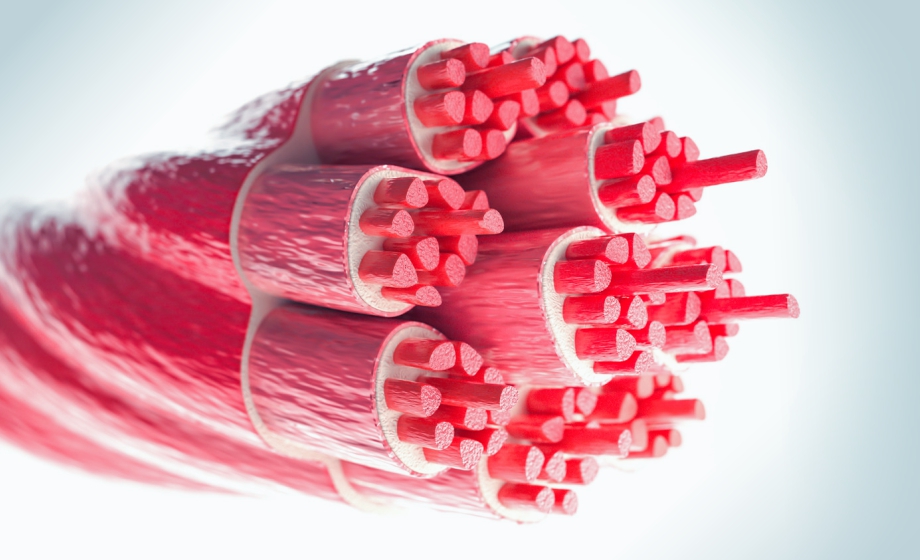
Is there a persistent loss/reduction of muscle blood flow/capillary network in these injured areas? Does this factor into the overall picture of failure to regenerate muscle function?
Vascularity and blood flow is one area that our group has not specifically evaluated. That said, it is expected that any approach to support regeneration of muscle fibers would require adequate regeneration of the vascular network.
Does movement affect the development of collagen in the muscle after an injury?
It is possible that initial loading is exacerbating the over-development of fibrosis, as the muscle needs to support loading for movement. In the model we use to the PT muscle, the duty cycle during standing and ambulation is low, so while the loading or movement after injury could be contributing to fibrosis it is unclear how significant this is to the overall development.
Can you make a distinction between movement and loading?
We have not evaluated loading, so I can not say for sure. That said, over the initial recovery period pigs are continually enticed to ambulate by both bout our research staff and the veterinary staff.
Is this applicable for muscle diseases such as muscular dystrophy or atrophy?
The key aspects of our work that are informative to other conditions, like muscular dystrophy, is how to understand limited regeneration of the muscle. For example, understanding mechanisms related to lack of metabolic improves after treatments could provide insight into how to improve metabolism in dystrophic muscle.
Can you comment on VML injury in aged (e.g., equivalent to ~60-yr old humans) animals and the ability to obtain aged large animals?
To date, we have not evaluated aged animals (rodents or pigs). Dr. Jeffrey Wolchok’s group has done some work with the aged rodents in the context of volumetric muscle loss (VML). For the ability to obtained aged pigs, I don’t have a clear suggestion on this but would warn about the growing size of pig over their aging trajectory.
In the metabolic situation, did you correlate mitochondrial dysfunction with decreased contractility measured in the muscle?
In our work mitochondrial dysfunction has been evaluated in a number of situations, including permeabilized muscle fibers and in vivo whole body metabolism.
Have you applied this type of functional analysis in porcine models of hindlimb ischemia or denervation?
Our work has primarily focused on physiology during development (e.g. PMID: 33782573) or trauma. That said there are other examples of functional assessments using this same platform (see the Aurora library at https://aurorascientific.com/resources/publications/).
How much movement and loading does your housing environment allow the animals? Is there a feasible way to enhance this without needed a lot more space?
The pigs in our studies have all utilized the standard IACUC/USDA space allotment. The animals do have space for ambulation about the housing.
Can you lace the scaffold with muscle cells from much younger, developing animals?
Absolutely, a number of groups have used cellular approaches in isolation or loaded into biomaterials. I like the idea of cells from a younger or developing donor as those should provide additional regenerative potential for recovery and regeneration.
Do your findings have relevance for loss of muscle mass with aging?
Our findings that provide mechanistic insight into the plasticity of the muscle remaining after VML could support interventions in the aged population as well.
How do you plan to communicate your results to the clinicians?
To date, we have worked with clinical colleges primarily in orthopedics and transplant surgery to share results. We also commonly interface with military physicians-scientists to share our work. As we continue to progress this work presenting at more clinical organization (e.g. Orthopedic Trauma Association) will continue to be imperative.
Any hypotheses on why your treatment that preserves neuromuscular junction (NMJ) isn't currently showing much benefit in neuromuscular function?
At this point we are needing to evaluate the function of individual NMJs (patch clamping for example) to understand if release kinetics or something similar is not adapting along with innervation. It could also be possible there is an over-activity of the muscle activity that is impacting function as recovery occurs.
Do you see changes in mRNA or microRNA expression in the damaged tissue that correlates with regeneration (or lack of)?
In collaborative work, we have evaluated sequencing profiles of the muscle remaining after injury and overwhelmingly there is an excessive increase in many myogenic signaling pathways. Significant work in this area is being done in the lab of Dr. Carlos Aguliar.
Most animal model research injures and treats at the same time. Regarding timing of therapeutics, is it possible to sustain the injured tissue first (maybe informed by your metabolic/fibrotic deposition data) and then deliver a therapeutic later, especially for sustaining nerve vs muscle fibers?
Yes, to date we have treated at the time of injury or the immediate day after. I think our data across rodent and large animals supports that starting treatment any time over the first two weeks could be beneficial. These delayed approaches are a current focus for our work.
Is there a difference in the sex of the animals in terms of recovery or response to VML injury?
At this point it is possible but not well evaluated in our group specifically. In a recent systematic-review and meta-analysis (PMID: 31578930) of various treatments for VML a pairwise sub-group analysis did not indicate a difference in treatment efficacy to promote functional recovery between male and female animals (mice, rats, pigs).
Have you used muscle stem cells for transplantation assays to study engraftment in the mini pig and if so, which reporter have you used for immunohistology?
The cellular therapies we have used are an endogenous minced muscle graft, to date. I know that immunohistochemistry can be challenging in the pig, please do reach out directly (grei0064@umn.edu) and I would be happy to talk through some options we have used recently.
Which are the more effective stressors for improving muscle hypertrophy after injury: metabolic or mechanical?
Our work would suggest that first improving metabolic function is necessary, then (or in parallel) mechanical loading is needed to drive hypertrophic improvements.